
Focused systems-wide suicide prevention efforts began at Kaiser Permanente (KP) in 2014, but gained traction in 2016 with KP’s growing awareness of the Zero Suicide framework and an interest in the significant outcomes demonstrated by other organizations in the health care industry. As one of the country’s largest integrated health care systems, implementing an organization-wide initiative of this magnitude has been a journey characterized by strong leadership support and collaborative, systemwide operational and data infrastructure development. These efforts have resulted in a core framework that allows for local adaptation, customization, and augmentation.
Key Success Strategies
- Systemwide agreement on a core clinical pathway for (1) identifying and treating patients at risk for suicide and (2) building electronic health record (EHR) tools to support the pathway
- Robust commitment from the organization to address significant data governance and infrastructure challenges to implement measurement strategy
- Continuous learning, ongoing evaluation and quality improvement, and integration into other national organizational priority focus areas
Background
Recognized as one of America’s leading health care providers and not-for-profit health plans, Kaiser Permanente currently serves more than 12.3 million members in eight states and Washington, D.C. Care for members and patients is focused on their total health and guided by their personal Permanente Medical Group physicians, specialists, and team of caregivers. The Permanente Medical Groups are self-governed, physician-led, prepaid multispecialty medical groups composed of nearly 23,000 physicians.
With industry research showing that many patients who die by suicide have had contact with the health care system in the months immediately preceding their death, KP made a commitment to identify suicide risk among their members and to respond effectively. As one of the country’s largest integrated health care systems, implementing an organization-wide initiative of this magnitude has been a journey that has been characterized by strong leadership support and ongoing interregional collaboration.
KP began its focused systems-wide suicide prevention efforts in 2014, and those efforts gained traction in 2016 with KP’s growing awareness of the Zero Suicide framework and an interest in the significant outcomes demonstrated by other organizations in the health care industry. A Zero Suicide AcademyÒ was held for the mental health leadership in all eight KP regions as well as the Permanente Medical Groups, which set a foundation for the work to come. With support from the KP’s national Care Management Institute, an interregional Suicide Prevention Learning Collaborative work group was formed. Participants included:
- Mental health leaders and champions from each KP region and Permanente Medical Group
- Risk management and patient safety partners from each KP region
- Researchers
- Key external collaborators and field experts
- Peer advisors (i.e., KP health plan members and advocates from national mental health advocacy organizations with lived experience)
The work group’s charter was to collaboratively develop processes and protocols to embed patient-centered, evidence-based suicide care in to standard practices, as well as to develop standardized metrics to ensure improved patient outcomes. The processes and protocols focused on the following areas, which align with specific Zero Suicide elements:
- Screening and assessment (Identify)
- Safety planning with lethal means reduction (Treat)
- Continuous monitoring and follow-up (Engage and Transition)
- Program evaluation and quality Improvement (Improve)
These efforts were bolstered by the establishment of an interregional mental health and addiction operational leadership group, comprising leadership members from all eight KP regions and Permanente Medical Groups. The group chose suicide prevention as a care delivery focus area and part of an overall national strategy for mental health and wellness, which led to an agreed-upon clinical pathway that all regions would work toward implementing, giving the organization a common goal, language, and data set.
Implementing the Clinical Pathway for Specialty Mental Health and Addiction Medicine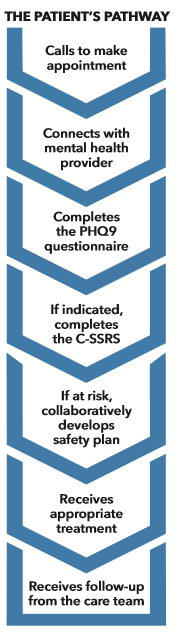
Although there may be some variance across KP regions and departments, screening is done using the Patient Health Questionnaire (PHQ-9) and the Columbia-Suicide Severity Rating Scale (C-SSRS). If the answer to the ninth question of the PHQ-9 is a 2 or 3, the C-SSRS is used as a follow-up screener to better identify the level of risk. A safety plan intervention is then initiated for patients whose C-SSRS score indicates a moderate or high risk of suicide.
A key element of implementation was building supportive tools in the KP electronic health record (EHR) system on a national level. The KP regions and Permanente Medical Groups were provided with the C-SSRS and the Stanley and Brown Patient Safety Plan Template to pull into their local EHR, which facilitates making the right thing easy to do. Additionally, blending suicide prevention with measurement-based care, another KP national priority initiative, helped support the fidelity of the screening model. For example, regional mental health and addiction services departments are moving to using tablet-based questionnaires, given at every visit, embedded with either universal screening using the C-SSRS (for teens) or automated flow of the C-SSRS from the PHQ-9 (for adults). The questionnaire data immediately flows to a dashboard, alerting provider(s) of any potential suicide risk.
Establishing Measurement Strategy and Metrics
Early on, it became apparent that implementing the measurement strategy on a national level would require robust commitment from the organization to address significant data governance and infrastructure challenges. These challenges included:
- Buy-in was needed from the Kaiser Permanente leadership from the eight regions and Permanente Medical Groups where KP operates.
- Acquiring death data to monitor suicide incidence required that data use agreements be forged with the different state vital statistics agencies in the states where KP operates.
- IT infrastructure development was necessary to reliably capture data on the completion of workflow components, such as suicide risk assessments and safety planning.
The leadership structure that was in place was key to getting needed regional executive sponsorship and widespread support and resources for implementing the national measurement strategy. Another important development was the formation of the suicide measurement advisory committee, composed of operational, research, and analytic specialists from the Permanente Medical Groups and chaired by a performance measurement specialist from KP’s Care Management Institute. The advisory committee provided guidance on the development of measurement specifications and offered support in identifying data resources.
“Our approach to suicide prevention needs to involve the humans and the system. Human caring and outreach are essential, but we need to make sure we do that systematically; that we identify everyone who is at risk and that we always offer effective interventions.”
Greg Simon, MD, MPH, Senior Investigator, Kaiser Permanente Washington Health Research Institute; Psychiatrist, Washington Permanente Medical Group
In 2016, KP began monitoring annual suicide incidence rates for each of its regions. For this metric, KP regional rates are reported along with respective statewide and national incidence rates for benchmarking purposes. Time trend and pairwise comparisons are made between the regional KP rates and their respective statewide rates to understand how KP’s performance is changing over time, both relative to the KP regions and to the states where the regions operate.
Recently, KP began reporting the quarterly performance for several additional metrics, including the following:
- Completion of risk assessment following a positive screen for suicide risk
- Intentional self-harm incidence rates
- Follow-up after an emergency department (ED) or urgent care visit for intentional self-harm
- The Healthcare Effectiveness Data and Information Set (HEDIS) measures for follow-up after an ED visit for mental illness or substance abuse
Monitoring of the safety planning intervention is expected to commence in the coming year, once use of the newly built safety planning template in our EHR becomes more routine. KP is still working on measurement and data infrastructure strategies for follow-up in order to operationalize agreed upon minimum standards of care for follow-up across regions, including both frequency of contact and active outreach for missed appointments. In addition, many regions are expanding on these core metrics to better understand the impact their regional processes are having on care delivery and outcomes for selected subgroups, as well as for their health plan membership as a whole.
Table 1. Suicide prevention metrics and reporting frequency
| KP Program-Wide Suicide Prevention Metrics | Reporting Frequency |
|---|---|
| 1. Suicide incidence rate | Annual |
| 2. Suicide risk assessment (C-SSRS) with elevated PHQ-9 in Specialty Mental Health & Addiction Medicine | Quarterly |
| 3. Safety plan development for members testing positive on C-SSRS | Quarterly* |
| 4. Follow-up for incomplete appointment among at-risk members | Quarterly* |
| 5. Intentional self-harm incidence rate | Quarterly |
| 6. Follow-up after ED visit or urgent care visit for self-harm | Quarterly |
| 7. HEDIS follow-up after ED visit with primary diagnosis for mental illness | Quarterly |
| 8. HEDIS follow-up after ED visit with primary diagnosis for substance abuse | Quarterly |
*Metrics pending or under development
Next Steps
Kaiser Permanente is committed to helping shape the future of health care. Founded in 1945, Kaiser Permanente has a mission to provide high-quality, affordable health care services and to improve the health of its members and the communities it serves. Care for members and patients is focused on their total health and guided by their personal Permanente Medical Group physicians, specialists, and team of caregivers.
The suicide prevention work began in KP’s Specialty Mental Health and Addiction Medicine Departments and laid a foundation for the spread into Primary Care and Emergency Medicine, two key settings for suicide prevention. That expansion will help KP work across the system to ensure members at risk of suicide are identified early and receive appropriate life-saving treatment.
As a learning health care system, KP’s research centers have partnered with the Mental Health Research Network (MHRN) and the National Institute of Mental Health (NIMH) to study the fidelity and outcomes of the Zero Suicide model implementation in five participating KP regions (grant number is U01MH114087). This five-year research project will evaluate systems-level suicide prevention practices and provide valuable insights to support continuous quality improvement efforts. Additionally, KP is exploring opportunity areas around operationalizing MHRN-led research on the use of predicative analytics in identifying and acting on risk indicator algorithms.
Authorship Details
- Cambria Bruschke, MSW, Senior Consultant, Mental Health & Wellness, Care Management Institute
- Jean Flores, DrPH, Principal Consultant, Evaluation & Analytics, Care Management Institute
For more information, contact Cambria Bruschke at cambria.bruschke@kp.org.