Lead
Lead system-wide culture change committed to reducing suicides.
Toolkit
Lead
Leadership and Zero Suicide
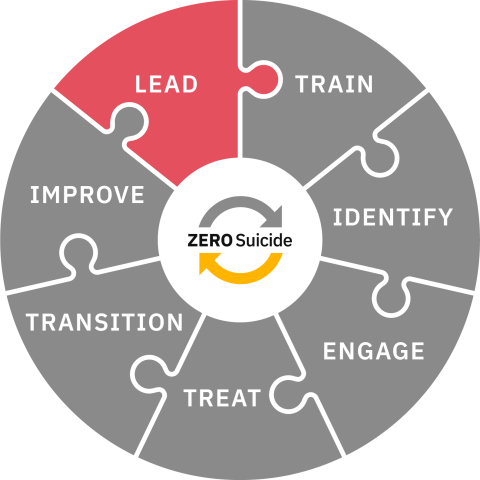
Organizational leadership is vital to the ongoing success of Zero Suicide implementation and is interwoven with every element of the framework. In Zero Suicide, the Lead Element represents a commitment that goes beyond one person, one leader, one department. This system-wide commitment is vital for the framework to take root and lead to sustainable systems-level changes and better quality care.
Implementing the Zero Suicide framework is not linear and will be specific to your organization, the services you provide, and the community you serve. To successfully implement Zero Suicide with fidelity, strength and commitment of leadership is required to determine the direction needed to best serve individuals at risk of suicide seeking support and healing from your care providers.
There are a few key areas in which leadership drives the dramatic reduction in suicide deaths achieved by organizations implementing Zero Suicide. The first is leadership mobilizing staff to truly believe that suicide can be prevented and that doing so is a system-wide priority that is the responsibility of every staff person. The second is an unwavering focus on the goal of reducing suicides — ideally, to zero. Leadership must both help staff see and believe that suicide can be prevented and provide tangible supports in a safe and blame-free environment — what is known as just culture.
Along the way, implementation will require that care providers change and adjust how they support individuals at risk of suicide using thoughtful safer suicide policies and processes at the organizational level. In order to achieve staff buy-in and support, the third key leadership area emerges as leaders at all levels make themselves available to listen, support, and reinforce the necessary changes to support suicide-safer care within their organization.
Zero Suicide calls for leaders to use opportunities to improve care driven by data, research and best practices, and feedback from staff, patients, and experts alike. Leaders must be prepared to tell the story of why Zero Suicide, why this organization, and why now so that staff members understand that Zero Suicide is not simply another healthcare initiative, but rather an evidence-based way of providing care that can help save lives.
In a Zero Suicide approach:
- Your organization has guidelines specific to suicide care.
- The guidelines emphasize the importance of the core components of safer suicide care, covered in detail in the seven sections of this Zero Suicide Toolkit:
- LEAD system-wide culture change committed to reducing suicides
- TRAIN a competent, confident, and caring workforce
- IDENTIFY patients with suicide risk via comprehensive screenings
- ENGAGE all individuals at-risk of suicide in a suicide care management plan
- TREAT suicidal thoughts and behaviors using evidence-based treatments
- TRANSITION individuals through care with warm hand-offs and supportive contacts
- IMPROVE policies and procedures through a continuous quality improvement plan
- The organization’s culture supports the well-being of all staff in tangible and accessible ways, with a commitment to do so spelled out within the guidelines. This support is made especially available to those doing hands-on work with those at risk of suicide. Care providers who are supported are better able to support others. Team members must be provided with the training, support, and guidance that empowers them to approach care provision with confidence and competence.
- There is ongoing communication with management and staff.
- Your CEO or another member of senior management conducts a presentation about the Zero Suicide philosophy, approach, and key elements to the board of directors.
- Your CEO and Implementation Team communicate the Zero Suicide philosophy, rationale, approach, and merits of this initiative to staff and establish a process for regular updates, at least annually.
- Changes as a result of your Zero Suicide initiative, including patient outcomes, are communicated to staff at all levels.
- Your implementation team provides management with training on the Zero Suicide philosophy, essential elements, and implementation plan.
- Leadership at all levels are empowered to provide staff with the support that they need to successfully improve how they provide care to patients, and steps are taken to ensure fidelity to the model.
- Your CEO and implementation team state a commitment to transparency and a no-blame culture when adverse events do occur.
Questions
What type of formal commitment have we made to reduce suicide and provide safer suicide care among people who use our organization’s services? Who will be the champions of Zero Suicide within our organization? Are those with lived experience of suicide attempt and loss in leadership and planning roles?
To Implement Zero Suicide
There are several important steps to take within the Lead Element that will prepare an organization to successfully implement Zero Suicide. While the framework is not meant to be linear in its implementation, the steps taken as part of Lead pave the way for every other element in the framework. Lead is a major touchstone for every other element and remains vital to the success of Zero Suicide at every turn.
Each section of the Zero Suicide Toolkit describes a core component of the approach, including specific features that organizational policies should contain.
Lead steps include:
- Establishing your Zero Suicide implementation team. The team is responsible for building and providing the foundation for your organization's Zero Suicide work. For more information about the Zero Suicide Implementation team, what team members should be in it, what their tasks are and will be, and their role as leaders within your organization, please visit the Implementation Team tab.
- Establishing the roles that those with lived experience will play, both on your implementation team and within your organization as Zero Suicide is rolled out. Individuals with lived experience play an important role in ensuring that an organization is suicide safe and person-centered in their services. As organizations establish themselves as committed to the goals of Zero Suicide, it is quite common for staff with lived experience to step forward as leaders. For a discussion of the vital role that those with lived experience play in Zero Suicide implementation, as well as the wide range of experiences that are important to consider, please visit the Lived Experience tab.
- Completion of the Zero Suicide Organizational Self-Study by members of your implementation team. You will use the results to determine priorities and set organizational goals. For more information and to view the self-study, please visit the Organizational Self-Study tab.
Zero Suicide and Responding to Organizational Staff Changes
Implementation of Zero Suicide is not a temporary initiative but, rather, a systems-level change in your culture around suicide care. It is vital that the guidelines that make up the framework for Zero Suicide implementation are structured in such a way that the success of the initiative is not dependent on one individual or even a small group of committed and passionate leaders and team members and, instead, takes root and flourishes system-wide. Zero Suicide must be baked into the core of your organization's approach to patient care so that responding to organizational turnover does not require a re-commitment to Zero Suicide and safer suicide care from the ground up. Staff turnover at any level can lead to a stall in progress and being prepared in advance with a plan to respond can help minimize impact.
In order to do so, your leadership and implementation team must consider documenting not only the guidelines that make up the foundation of your organization's Zero Suicide implementation but also those positions that are responsible for ensuring fidelity to the model and communicating your organization's culture and commitment around safer suicide care to new employees in all departments, including leadership. Some ways to do this might include:
- At the executive leadership level:
- Board members share their commitment to Zero Suicide and consider the framework important to the organization's vision and future.
- As new leaders are brought on, they are introduced to (and agree to support) the organization's ongoing commitment to safer suicide care through the Zero Suicide initiative. If possible, this is discussed as part of the hiring or selection process.
- The implementation team has created, with contributions from current leaders, guidelines for how leaders at this level can be onboarded to support safer suicide care through Zero Suicide while leaving room for new leaders to innovate in ways that support implementation.
- The steps to becoming informed are laid out in the guidelines, including who is responsible for providing support to new leadership in understanding the Zero Suicide framework and being brought up to speed on its progress. Ideally, this should involve leaders at all levels who are able to provide an overview of their team's responsibilities, progress, challenges, and successes.
- At the administrative and management level
- HR is engaged to ensure that values related to safer suicide care through Zero Suicide are built into job descriptions and new employee orientation. Your Zero Suicide implementation team can also work with HR to map out ongoing training requirements based on role. Institute for Family Health developed a training policy and crosswalk with job descriptions available on our website here.
- Administrative and managerial applicants understand from the beginning that Zero Suicide is part of the organization’s culture. This starts with mentioning the organization’s commitment to safer suicide care from the start and building it into hiring processes and tools. As a result, new leaders understand from the start the roles that they, as well as their teams, play in providing safer suicide care to individuals in care.
- Champions of Zero Suicide at all levels have the opportunity to meet with new leaders and orient them to the framework.
- Team members are provided with the opportunity to meet with new leaders and discuss their experiences with carrying out Zero Suicide with individuals in their care, including what has gone well, those things that have been challenging, and feedback for team-level improvement.
- New leaders are provided with written guidelines for their role, and that of their team, within Zero Suicide implementation that have been prepared by the Implementation Team, with feedback from the previous leader, if possible.
- New leaders understand that everyone has a role to play in providing safer suicide care, and that, in supporting their team members in their successes and challenges, the organization operates within a just culture approach and how this is operationalized.
- At the team level:
- Applicants for all roles understand from the beginning of the employment process that one of the organization’s goals is to have zero suicides among individuals in their care. Applicants understand what is means to operate within a just culture and that everyone in the organization has a role to play in providing safer suicide care.
- New team members have a clear understanding of their role within their team in the context of Zero Suicide and are provided with the training and support required to approach these responsibilities with confidence and competence.
- There is a clear understanding of how team members can seek out support from their leaders, whether in the context of providing care to individuals seeking services, or because they themselves are in need of support.
- There are written guidelines for onboarding new team members to the Zero Suicide framework that have been created in-line with the responsibilities of the team and role. These guidelines were created by the Implementation Team with feedback from the team so that they are specific and clear.
Integrating Zero Suicide with other Healthcare System Initiatives
The Zero Suicide framework need not stand on its own or cancel out the implementation of other important initiatives in healthcare. While the goal and approach of Zero Suicide is unique, the focus on providing evidence-informed care in an environment where safety, accountability, compassion, and respect are priorities is not. There are many healthcare initiatives with which Zero Suicide integrates, and, in doing so, the implementation of each initiative is strengthened.
Mike Hogan, co-chair of the Zero Suicide Advisory Group of the National Action Alliance for Suicide Prevention, talks about applying the core concepts of the patient safety movement to prevent suicide:
Implementation Team
Establish a Zero Suicide Implementation Team
One of the most important early steps of your Zero Suicide journey is the establishment of a Zero Suicide Implementation Team. An organization’s Implementation Team is responsible not only for the first steps of implementation but also for the ongoing development and updates of goals and guidelines, and continuous quality improvement in response to feedback and data.
In many ways, the success of implementation relies on an implementation team that is committed to Zero Suicide and where each member understands their role within the organization and team and is prepared to be a champion of the initiative. It is critical that the responsibility of the initiative does not fall to only one person. Zero Suicide implementation requires a multidisciplinary approach with team members from various areas of the organization (e.g., those providing care, leadership, data, legal).
Tasks, Roles, and Responsibilities
- A Zero Suicide implementation team is established with the charge, tasks, and roles of members clearly defined, including:
- A schedule for regular team meetings
- Authority for developing and changing guidelines as needed
- An evaluation plan designed to assess the impact of the initiative
- Responsibility for continuous quality improvement and the development of specific approaches to measuring and reporting on all suicide deaths
- The implementation team includes as partners individuals who are prepared and eager to serve as champions for the initiative
- The suicide bereaved and those with lived experience are part of the Implementation Team and participate in some or all of the following activities:
- Providing regular input and advice
- Assisting with workforce hiring and/or training
- Participation in evaluation and quality improvement efforts
- Participation in multiple aspects of suicide care
- The Implementation Team completes a Zero Suicide Organizational Self-Study for baseline information and uses the results to set organizational goals. The Implementation Team should also set up an annual retaking of the Self-Study to track progress and as a fidelity tool.
- Ideally, the Implementation Team has a budget to support Zero Suicide implementation. Many organizations, however, are only able to dedicate staff time to implementation. Implementation Teams should think creatively about the resources needed to achieve their goals – resources that include staff time, training funds, IT and EHR updates, etc.
- The Implementation Team explores ways to link Zero Suicide to other initiatives, such as trauma-informed care or substance abuse prevention and treatment programs.
- The Team reviews all of the organization’s policies to determine what new policies need to be developed. Policies and procedures include:
- Approaches to measuring and reporting on all related process (e.g., screenings, assessments, safety plans developed) and outcome (i.e., suicide attempts and deaths) measures. See Data Elements Worksheet.
- Supports provided to staff that have experienced suicide death of a client
- Suicide care planning and tools are embedded in the electronic health record
- Staff are trained on use of the electronic health record to track clients at risk for suicide.
Implementation Team Members
In building the organization’s Zero Suicide implementation team, it is important to consider the scope of the responsibility tasked to them. Implementation team members should be in a position where they have in-depth knowledge of the tasks and responsibilities of their departments, are experienced with making decisions related to guidelines and procedures, and are committed to the continuous quality improvement that is foundational to the success of Zero Suicide.
Team members should come from a variety of departments reflective of the principle of Zero Suicide that everyone in an organization has a role to play in providing safer suicide care. Together, members of the implementation team can speak to what has been standard care, what may be possible, and what it is likely to take to achieve the improvements discussed throughout Zero Suicide. Implementation teams should, at minimum, include leaders and representatives of the following departments, as applicable to the organization:
- Leadership: By involving high-level leadership, communication between those responsible for the executive leadership of the organization and those on the implementation team will be ensured. Executive leadership can be the voice of the organization’s vision and values, and act as a champion of the initiative with the other members of the executive leadership team, including the board. They can help secure resources and ensure the participation of necessary departments in your organization.
- Administrative: Those on the administrative side of the organization’s operations, including departments such as Human Resources, Finance, Operations, and Admissions, can help to provide information related to hiring, policies and procedures, cost, and impact on patient admission. Especially important to a just culture is working with Human Resources to understand how to provide non-punitive support, remediation, and care to employees who lose a patient so suicide. They can speak to what is possible on the administrative side of the organization, as well as help to integrate Zero Suicide into their respective departments and work with their team members to understand what their roles and responsibilities are within the initiative (e.g., training staff in finance how to connect individuals who are in distress during calls about billing to appropriate screening and care).
- Clinical: Those providing the hands-on care to individuals seeking services from your organization are critical to the success of your Zero Suicide initiative. These team members can speak to the impact of various new standard practices on the individuals they serve, as well as clinical discussions around evidence-based and evidence-informed practices that are, or may be, implemented. They can also make sure that the voices of their colleagues and staff are heard and that concerns can be addressed and solved.
- Peer services staff: For organizations that have peer services, involving staff from this area can provide a great deal of insight in terms of care that would be received and perceived as helpful, respectful, and collaborative. Peers are often considered as extremely important members of care teams due to the connection they have with those currently seeking care; they have been in a similar place, perhaps dealt with similar concerns, and can offer guidance and support that other care providers may not be able to simply due to a difference in life experiences. For many individuals at risk of suicide, being supported by a peer can offer a great deal of comfort with the organization’s services during a time when it is especially important.
- Individuals with lived experience and expertise: Individuals with lived experience in surviving suicide attempts and ideation can provide a perspective that is vital to Zero Suicide implementation. Including those with lived experience can help the other members of the implementation team understand what may be harmful, what would be helpful, and ways of communicating care with individuals at risk of suicide that is supportive, safe, collaborative, and respectful. For more information on involving those with lived experience on implementation teams, look at the Lived Experience tab (above in the LEAD element toolbar).
- Legal/risk management: It is likely that changes made to the care of patients and clients seeking care from the organization will require approval from the legal department, especially regarding interventions that may require changes to informed consent documents, discharge procedures, and others. Examples of the type of interventions that may involve changes to consent documentation are consent from individuals in care to contact them post-discharge, consent to involve support persons such as friends and family in care, and consent to contact other providers involved in the individual’s care, among others. Implementation team members from legal departments can make sure that consideration is made to patient care privacy laws, liability, and other concerns that may arise in the course of Zero Suicide implementation. Legal professionals can help draft the guidelines that support changes to patient care and make clear the rights and responsibilities of all involved.
- Quality Assurance: Having members on the implementation team with thorough knowledge of data collection, analysis, and continuous quality improvement can strengthen every step of the IMPROVE element of Zero Suicide implementation and help to ensure that evaluation plans are solid from the start. They can assist in the process of determining adjustments that may need to be made to achieve the desired results and fidelity to the model, as well as determining the measures that will most accurately reflect the impact Zero Suicide implementation within the organization. Similarly, QA professionals can help determine the tools that are available for data collection and the best way to utilize the resources that the organization has to best optimize results.
- Information Technology: The major aspect of the ENGAGE element is the development of a care pathway that allows providers to ensure that individuals at risk of suicide or provided with the suicide-specific care best optimized to support them. In order to do so, many organizations collaborate with their IT departments on creating systems, most frequently via an electronic health record, that allows for an integrated approach to the care pathway. Involving IT professionals on the implementation team can allow a more thorough understanding of what is possible and how best to utilize the technology that is available to the organization, as well as the most clear and efficient ways of training staff in its use.
- Support staff: Support staff are incredibly important to the implement team due to the frequency with which they have contact with individuals seeking out care from the organization. Oftentimes, individuals at risk of suicide will disclose issues they are going through to those with whom they are most comfortable, and that person is not always a care provider in the traditional sense. Support staff includes, but is not limited to:
- Those individuals responsible for making appointments and greeting those seeking care, such as medical receptionists
- Custodial staff who are in frequent contact with individuals seeking care, especially individuals who have been admitted to the hospital for longer lengths of stays
- Discharge planners
- Patient care advocates/ombudsmen
- Billing and finance staff who field calls about medical bills
Organizational Self-Study
Taking the Organizational Self-Study
The Zero Suicide Organizational Self-Study is designed to allow you to assess what core elements of safer suicide care your organization currently has in place. The self-study can be used early in the launch of a Zero Suicide initiative to assess organizational strengths and weaknesses and to develop a work plan.
While the self-study is not exhaustive with regard to all issues that can affect patient care and outcomes, it reflects the core components that define the Zero Suicide comprehensive approach. The organization’s Zero Suicide implementation team should complete the self-study, with input from staff involved in the creation of foundational guidelines and care for patients at risk for suicide.
There are a variety of ways for the implementation team to conduct the self-study, depending on the type and size of the organization. For example, a large, multi-site organization might ask the leader of each geographic location to complete the self-study for that location. The results could inform individualized planning for each location and at the same time suggest actions that the corporate leadership may need to take.
Since each member of the implementation team will likely be the leader of a significant area of the organization, another option is to have all the team members complete the self-study. A designated team member could consolidate the ratings, which could be a starting point for a discussion of goal setting and work plan development. Alternatively, the team might complete one self-study together, coming to a consensus on each item.
Accessing the Organizational Self-Study
We strongly encourage you to log in and use the online portal to input your data. Using the portal will give you access to a report and annual reminders to retake it as a fidelity tool.
For Tribal or IHS-Led Health Systems, we offer an Organizational Self-Study Addendum.
The Zero Suicide Organizational Self-Study is available in four versions:
- General Organizational Self-Study. This version is designed for systems with multiple departments, outpatient behavioral health settings, integrated treatment for co-occurring disorders, primary care, FQHCs, and other settings that provide care and services to individuals at risk for suicide.
- Inpatient Organizational Self-Study. This version is designed for organizations that have a primary focus on inpatient health and behavioral health care. These may include more intensive levels of care—such as partial hospitalization—or intensive outpatient programs if managed under the inpatient organizational structure.
- Community-Based Organizational With Clinical Providers Self-Study. This version is for community-based organizations that employ health and behavioral health care providers (e.g., correctional facilities, homeless-serving organizations, and elder care organizations) and are working in partnership with health systems to implement Zero Suicide.
- The Community-Based Organizations without Clinical Providers Self-Study. This version is for community-based organizations that do not employ health and behavioral health care providers (e.g., correctional facilities, homeless-serving organizations, and elder care organizations) and are working in partnership with health systems to implement Zero Suicide.
Lived Experience
What do we mean by Lived Experience?
There are many ways we talk about lived experience in suicide prevention and the Zero Suicide Toolkit. A few you'll see in the Zero Suicide Toolkit include1 :
- Lived experience: A broad term encompassing a range of experiences with suicidal intensity. This range includes direct and personal experience of suicide as well as experience of the personal impact or trauma related to a suicidal crisis within one's social circle.
- Personal lived experience of suicide: Firsthand experience with suicidal thoughts, feelings, and/or intensity. This category includes surviving a suicide attempt as well as ongoing or intermittent suicidal experiences.
- Relational lived experience of suicide: Experience from being close to someone who went through (or is going through) suicidal intensity. This category includes bereavement from suicide death as well as experience as a close friend or family member of someone with personal lived experience of suicide.
- Lived expertise: The combination of role-relevant skills and knowledge based in lived experience that is used to advance suicide prevention structurally, through introduction of lived experience learnings in program design or implementation, policy or organizational practices, research design and application.
- Peer support: Any support provided by one person to another that relies on shared experience, especially the shared experience of adversity. Peer support may be informal, mutual, or highly structured in the form of a professional service (e.g., peer support services).
- Peer specialist: Someone employed to provide professional peer support services, most often in the domain of behavioral health and recovery. Peer specialists normally have substantial training prior to employment although these trainings vary. In most U.S. states, peer specialists are required to obtain certification in order to provide services.
Involving People with Lived Experience
For an organization implementing Zero Suicide, one of the first actions should be to partner with people with lived experience in developing, implementing, and evaluating efforts. For example, your Zero Suicide implementation team should include at least one person with lived experience. Including those with lived experience provides many valuable and impactful benefits that support your organization’s success with Zero Suicide implementation: most importantly, providing high-quality, compassionate, and collaborative care to those individuals at risk of suicide.
Amplifying the voices of those with lived experience can allow your organization to better understand the impact of your services and create a system of care in which individuals feel respected, heard, and safe. Additionally, by consulting with those with lived experience as a loved one of an individual with suicide risk, as well as those who have experienced suicide loss, your organization can build a system of care that takes into account the vitality of support networks while also respecting the privacy of those in care.
Similarly, by creating an opportunity for those who are in care, or those who have previously been in care, to share their feedback, your organization makes clear that they are committed to patient-centered care and are eager to learn how they can provide better support to individuals at risk of suicide. You may not have to look outside your organization for lived experience. Many organizations find that they have staff with lived experience. Clinical practice often discourages self-disclosure to avoid harm to patients and therapeutic relationships. Including individuals with lived experience as part of your implementation team is something different and of significant importance.
Suggestions for Involvement
Engaging People with Lived Experience: A Toolkit for Organization offers guidance on recruiting and engaging individuals with lived experience inside and outside your organization. Other key areas outlined in the toolkit for organizations are how to ensure that involvement is beneficial to them and the organization as well as what meaningful levels of engagement are based on your organization's needs and the desire of the individual with lived experience.
The Suicide Attempt Survivors Task Force of the National Action Alliance for Suicide Prevention issued a report - The Way Forward: Pathways to Hope, Recovery, and Wellness with Insights from Lived Experience - that offers a set of core values to inform suicide prevention and care as well as specific recommendations for health and behavioral healthcare organizations and program developers.
The Way Forward suggests several ways in which people with lived experience can be involved in improving suicide care:
- Suicide prevention and behavioral health care organizations can engage, hire, and/or collaborate with peer support professionals. They should also include attempt survivors as key partners in suicide prevention and safer suicide care efforts.
- Providers of crisis or emergency services can develop formal partnerships with organizations that offer peer support services and especially organizations that are operated or driven by people with lived experience.
- Suicide prevention and behavioral health groups can engage attempt survivors as partners in developing, implementing, and evaluating efforts.
- All types of providers can use a certified peer specialist on care coordination teams. This involvement can have direct benefits for a person receiving care, including role modeling and improved problem-solving.2
Recommended Resources
- 1We'd like to thank DeQuincy Levine, Ph.D., for sharing these definitions.
- 2National Action Alliance for Suicide Prevention, Suicide Attempt Survivors Task Force. (2014). The way forward: Pathways to hope, recovery, and wellness with insights from lived experience. Washington, DC: Author. Retrieved from https://theactionalliance.org/resource/way-forward-pathways-hope-recove…
Next Steps
Create a Leadership Culture for Safer Suicide Care
Are you ready to implement safer suicide care through Zero Suicide in your organization? If so, the next steps to create a leadership culture that supports safer suicide care are:
- Review the online Zero Suicide Toolkit.
- Challenge your organization to adopt a comprehensive suicide care approach using the readings and tools in the Lead section of the toolkit.
- Convene your Zero Suicide implementation team.
- Discuss and complete the Zero Suicide Organizational Self-Study, provided in the Tools below.
- Create a work plan and set priorities, using the Zero Suicide Work Plan Template, provided in the Tools below.
- Create a plan to collect data to support evaluation and quality improvement, using the Zero Suicide Data Elements Worksheet, available in the IMPROVE section of the toolkit.
- Announce to staff the launch and adoption of an enhanced suicide care approach.
- Use the Getting Started with Zero Suicide resource to learn the first steps to take to adopt this comprehensive suicide care approach.
From an Implementer
In this short video, Zero Suicide Institute faculty members Dr. John Ackerman and Dr. Glenn Thomas describe Nationwide Children's Hospital's experience implementing Zero Suicide, highlighting key success factors such as strong leadership support, focused tools and training for clinical staff, a well-established quality improvement infrastructure, and the input of clinicians from across the hospital and individuals with lived experience: