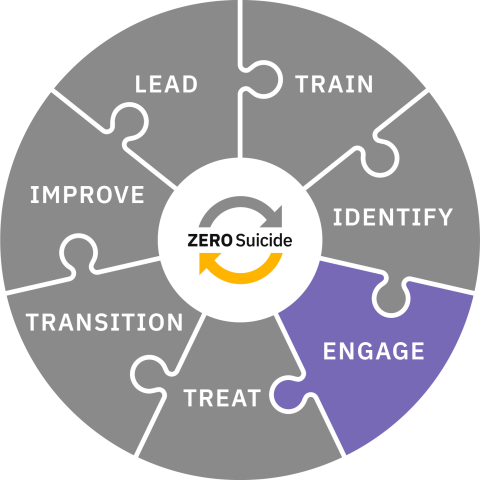
Engage
Engage all individuals at risk of suicide using a suicide care management plan.
Toolkit
Engage
Engaging Individuals at Risk
When an organization makes a commitment to Zero Suicide, every individual who is identified as being at risk for suicide is connected to collaborative care and support. They are engaged continually during every encounter through specific steps and interventions; this occurs regardless of the reason for the individual's visit.
This series of steps to maintain continuous engagement and ensure high-quality care is called a pathway to care.
The prioritization of a collaborative and engaging approach to safety is a core tenant of the Zero Suicide approach, ensuring that every individual at risk for suicide is an active participant in their own care. The Engage element emphasizes the simultaneous importance of evidence-based systems of support and individual autonomy and self-expertise.
In a Zero Suicide approach, Engage broadly refers to:
- A pathway to care that instills hope and is recovery focused
- Collaborative safety planning
- Counseling on access to lethal means
- The steps taken by providers to maintain the patient's engagement in, and commitment to, their care while working collaboratively with the individual
- Maintaining communication with the individual between appointments and during transitions
- The pathway is embedded and documented in an electronic health record
- Supporting healthcare workers who provide the care for individuals at risk of suicide
Providers and Processes
The success of the care delivered to individuals at risk for suicide in the Treat and Transition elements of the Zero Suicide framework relies heavily on the work done by providers within the Engage element. The efforts put forth by providers to provide collaborative, compassionate, and evidence-based care create an environment in which the individual feels their voice is heard, they are cared for, and they are supported and empowered in getting their needs met during their care and recovery.
Organizations that have reported the most success in providing individuals with a pathway to care use the electronic health record (EHR) to flag individuals at risk of suicide so that providers are aware of the potential need for additional support around suicide risk.
By using the EHR, care becomes more streamlined and consistent, and the frequency with which individuals must start from the beginning with providers or organizations is decreased; the provider and individual are on the same page and know what to expect. Within the EHR, a provider can find information related to the individual's risk, information on their safety plan, and other providers who are part of the care team.
Questions
What is our approach to following the care of individuals at risk for suicide?
How will we provide care that engages individuals at risk of suicide and empowers them in their recovery?
How are those with lived experience engaged in the process of establishing collaborative engagement practices?
What formal review processes will be implemented to ensure individuals have felt engaged, heard, and empowered?
Design Suicide Care Management Guidelines
Design guidelines for engaging a patient in a pathway to care, which should specify the following:
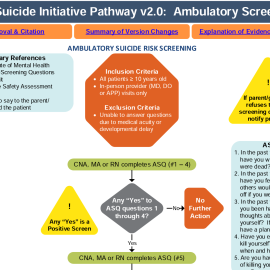
- The screening tool and criteria to indicate that the individual should be engaged in a pathway to care
- Provision of same-day access to a behavioral health professional for formulation of a clinical judgment of risk using a standard risk formulation framework
- Requirements and protocols for safety planning, crisis support planning, and lethal means safety
- The frequency of visits for a patient on a suicide care pathway
- Actions for the provider and system to take when an individual misses an appointment or stops engaging in care as well as educating individuals on those steps
- The process for communicating with an individual about their diagnosis, treatment expectations, and what it means to be on a suicide care pathway
- Parameters for continued contact with and support for the individual, especially during transitions in care
- The referral process to suicide-specific, evidence-based interventions
- How documentation of progress and symptom reduction will take place
- Criteria and protocols for closing out the suicide care pathway when an individual is ready
Implement Suicide Care Management Policies
Change systems and get staff buy-in so that policies will be followed by:
- Establishing use of the EHR to monitor individuals in a pathway to care
- Training all staff in use of the relevant features of your EHR related to the care pathway (e.g., assessments, safety plans, ways to ensure warm handoffs, caring contacts)
- In the absence of an EHR, ensuring all staff clearly document individual status and updates in the paper record
- Training staff on discussing the meaning of a pathway with individuals who are placed on one, as well as what the individual can expect moving forward with special emphasis on engaging and instilling hope
- Training all staff at least annually in your organization's care pathway guidelines and protocols so they know what is expected of them, the philosophy behind these policies, and how they will be supported by the system
- Establishing a schedule for regular team meetings and clinical case consultations to discuss individuals at risk.
- Setting a schedule for management to regularly review charts to determine that policies and protocols are being followed not just in letter, but also in the spirit of instilling hope
Implementing these suicide care management policies can be supported by using your electronic health record (EHR) and many systems have found the EHR to be a key factor in constantly engaging individuals at risk for suicide in a pathway to care.
Healthcare Worker Wellness
Health and behavioral healthcare workers are experiencing burnout at high rates and organizations have to develop ways to support their workforce so they can provide the needed care to those individuals at risk of suicide. There are many toolkits and recommendations from government and non-government agencies like the U.S. Surgeon General, SAMHSA, the World Health Organization, Institute for Healthcare Improvement, and the American Medical Association. All of these, and more, can be found in the resource section of this toolkit.
Rationale for EHRs
Health and behavioral health organizations should take steps to ensure that a patient’s suicide risk is reviewed at each visit and that care is coordinated and communicated between the patient and professionals within and outside of the organization.
Building the capacity to follow the care of patients at risk in an electronic health record (EHR) system can help ensure that care is continuously, consistently, and deliberately provided by all involved to address suicide risk. However, not all organizations have a comprehensive EHR system. Nevertheless, every organization should attempt to record suicide screening results, risk formulation, and suicide-specific care plans in each patient’s record. Paper records should be reviewed periodically to ensure that suicide risk is being assessed and recorded by each staff member designated to do so.
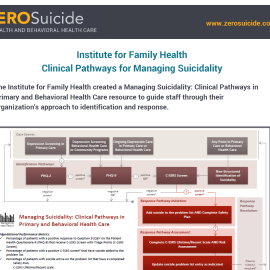
Implementer Example
The Institute for Family Health (IFH) is one organization at the forefront of using the EHR in service of a Zero Suicide initiative and providing safer suicide care. Perhaps the most important advice from IFH’s experience is to include someone from the organization’s information technology (IT) department on the Zero Suicide implementation team from the very beginning. Involving an individual from the IT department of your organization will make sure that you are informed about what is possible and are able to create buy-in within the department as you work together closely to build out the EHR in such a way that the care pathway can be integrated and easily accessible.
The video below describes how IFH modified their EHR to support better safer suicide care management.
Engaging with Individuals via Telehealth
Telehealth has become a vital part of the health and behavioral healthcare service delivery system. For many providers accustomed to face-to-face patient interactions, there may be questions about the best way to engage with patients via the telephone and/or video contacts. Some individuals may prefer telehealth visits for several reasons, ranging from those related to personal comfort to those having logistical concerns. There are many ways to provide excellent and compassionate ongoing care via telehealth that allow the provider to screen and assess for suicide risk, collaborative create safety plans, provide counseling on access to lethal means, and provide urgent care to those who require it. We have many resources available to providers regarding providing various aspects of care via telehealth by visiting the Telehealth section of the Providing Suicide Care During Covid-19 page.
Watch the video below for a short video about how one Brave Health clinician overcame their fears about telehealth.
Pathway to Care
Continuous Quality Care
When individuals are at risk for suicide, a pathway to care can be instrumental in working with them to feel safe, secure, and able to stay alive. A pathway to care is a predetermined series of steps to maintain continuous engagement and ensure high-quality care for these individuals. Your organization will need to create a pathway unique to your system, utilizing internal and local resources.
Organizations implementing a pathway to care approach should consider the following to develop your own unique pathway.
In a Zero Suicide approach:
- What services does your organization offer to individuals?
- What referrals or transfers of care will or could happen based on potential progression of risk?
- Who will your organization communicate and coordinate with regarding the individual's care (e.g., primary care, outpatient providers, emergency contacts)? What releases of information and/or MOUs or agreements will be needed to do so?
- How will your organization follow-up with the individual? What contact information is needed to do so?
- How soon after the initial assessment will your organization meet with the individual at risk again?
- What protocols exist within your system if the individual does not come to the follow-up meeting?
- How do staff address lethal means safety with the individual?
- How are the voices of people with lived experience being incorporated into the development of your suicide care pathway?
Outlining a Pathway
An effective pathway to care creates a sense of direction for both the individual at risk and the provider. It can help a provider remain clear and steady during a suicide evaluation and increase the trust the individual has in the system’s competence and compassion. As such, it is important that each organization’s pathway to care is clearly and carefully outlined for both staff and the individuals they serve.
Clear documentation should be provided to anyone on a pathway to care explaining what it is, what they can expect, and who they can contact. Evidence shows that individuals at high risk of suicide are often among the highest percentage of those who drop out of treatment; a clearly established pathway can increase the likelihood of the individual remaining engaged.1
Assuring all staff are not only informed of pathways to care but properly trained in their use is a necessary step for proper implementation. Organizations should provide initial trainings in pathways for staff members, as well as hold regularly scheduled refresher trainings. Measures should be in place to ensure providers feel confident and capable to use a pathway to care effectively.
Electronic Health Record
Processes for documenting the established pathway to care and takeaways from the conversation with the individual into an electronic health record (EHR) should be clearly laid out for staff.
Further, staff beginning work with an individual they have not worked with previously should become familiar with reviewing charts within the EHR for information on their pathway to care. Promoting consistent and effective use of an EHR promotes a uniform treatment plan and reduces an individual’s need to repeat themselves.
Lived Experience
As is true for all elements of the Zero Suicide framework, it is imperative that voices of lived experience are involved in the creation and implementation of the pathway to care. People who have experienced suicidality should be actively engaged in creating what the pathway includes, what language is used, how staff are trained, and how to engage with individuals. As the organization implements and periodically reviews its use of the pathway to care, people with lived experience should be at the center of the conversation throughout. Similarly, as part of active engagement, as individuals at risk for suicide find increased stability, their input on the pathway to care based on their own reactions and perceptions should be incorporated.
Active Engagement for Safer Suicide Care
A fundamental premise of the Zero Suicide approach is that safer suicide care begins from the moment the patient calls the organization for an appointment or is admitted for treatment. For example, suicide risk immediately becomes a primary focus of assessment in a behavioral health or primary care setting if a patient indicates that he or she is currently having suicidal thoughts, has had suicidal thoughts in the past, or has made prior attempts.
Another fundamental premise is that all staff members have a crucial role in preventing suicide. Suicide risk should be assessed collaboratively, compassionately, and frequently with patients who are at risk of suicide. The frequency of assessment may depend on a number of factors specific to your organization and patient populations, however, all providers should be aware and prepared to collaborate with the patient around their suicide risk. This attention to individuals at risk for suicide by all staff members, clinical and non-clinical, requires a fundamental shift in what a health or behavioral health organization sees as its role.
Although a great deal of the focus of Zero Suicide is keeping patients safe from harm, engaging patients is not solely about making sure that they come in for visits. The goal is for patients to grow, gain skills, and recover. The patient and provider relationship and rapport plays a major role in the disclosure of suicide risk by the patient and their subsequent engagement in their care. Care that is compassionate, empowering, and strengths-based builds on the trust between provider and patient can help to support the patient on their path to recovery. Further, care does not begin and end only within the time spent with the patient face-to-face in care, but also involves contact between visits when needed, as well as during transitions in care.
Actively engaging a patient about suicide risk:
- Takes into account the individual’s experiences and resources and gives them a voice in their care
- Builds hope for recovery
- Empowers the individual to resolve crises and long-term problems using the least invasive methods possible
The result of active engagement in suicide care is that the patient feels heard, cared for, and empowered to make safe decisions.
Care that focuses on suicidal thoughts and behavior may be new and even overwhelming to a patient and family. The collaborative, nonjudgmental, comprehensive approach that is part of Zero Suicide may be a very different experience for many patients with suicide risk, especially if prior treatment has failed them. Staff members will need to take care to let patients know what to expect and guide them in how to use treatment effectively.
As you are planning your implementation of the Engage element, consulting with your implementation team members with lived experience regarding the best ways to do this will allow your organization to implement guidelines and standard care practices that meet the goals set forth within this element.
Caring Contacts as Non-Demand Engagement
One evidence-based way to supportively engage individuals is the use of non-demand caring contacts. These contacts are brief communications that are non-demand (meaning they don't ask the individual to do something) and show support. Research has found that this low-cost and scalable intervention can have significant effects on an individual. Not only can they promote connection to care and increase their participation in collaborative treatment, caring contacts have also been shown to decrease reports of suicidal ideation and suicide attempts compared to the standard of care in a wide variety of health and behavioral healthcare settings.2, 3, 4
The use of caring contacts can help engage and re-engage individuals in care when they miss appointments, choose to stop treatment, and during care transitions or discharge from care. They may be especially helpful to individuals who have barriers to care or are unable or uninterested in accessing treatment.
As part of your care pathway for individuals at higher risk of suicide, it's critical to consider the populations you serve, the channels through which individuals prefer to receive communication (texts, letters, emails, care portal messages) and the content of the messages.5 For more information about caring contacts and examples of caring contacts from a variety of systems, visit the Transition element.
Suggested Resources
Care Pathway Resources
Sample Care Pathways
Other examples of care pathways are available in the resources section.
- 1Stanley, B., and Brown, G.K. 2012. Safety planning intervention: A brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256-264.
- 2Comtois KA, Kerbrat AH, DeCou CR, et al. Effect of Augmenting Standard Care for Military Personnel With Brief Caring Text Messages for Suicide Prevention: A Randomized Clinical Trial. JAMA Psychiatry. February 2019.
- 3Luxton, D. D., June, J. D., & Comtois, K. A. (2013). Can postdischarge follow-up contacts prevent suicide and suicidal behavior? A review of the evidence. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 34(1), 32.
- 4Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52(6):828-833.
- 5Reger, M. A., Luxton, D. D., Tucker, R. P., Comtois, K. A., Keen, A. D., Landes, S. J., Matarazzo, B. B., & Thompson, C. (2017). Implementation methods for the caring contacts suicide prevention intervention. Professional Psychology: Research and Practice, 48(5), 369–377.
Lethal Means Safety
Access to Lethal Means
Reducing access to lethal means, such as firearms and medication, is a critical component of suicide prevention. Studies from around the world have demonstrated that the overall rate of suicide drops when access to commonly used, highly lethal suicide methods is reduced.1, 2, 3
In the late 1950s, the United Kingdom switched from coal gas to natural gas, which is free from carbon monoxide. Suicide deaths decreased, saving thousands of lives over the next 10 years.1 A study in Australia found a decrease in suicide by firearms and in the overall national suicide rate following a 1998 ban on private gun ownership.3 While these studies demonstrate the importance of advocating for means restriction on a larger, policy-based scale, they also translate into the individual level—removing access to lethal means can save lives.
Research has shown that among people who made near-lethal suicide attempts, 24% reported taking less than five minutes between the decision to kill themselves and the actual attempt; 70% took less than an hour.4 Based on this evidence, it is clearly possible to increase the chance of surviving an attempt if an individual at risk for suicide has reduced access to lethal means in their moment of crisis.
CALM Training
This can be one of the most challenging tasks a clinician faces in suicide care. The Counseling on Access to Lethal Means (CALM) online training is offered free of charge through the Zero Suicide website as one tool to address providers’ preparedness in handling this difficult area of care.
Research shows that mental health providers demonstrated an increase in knowledge and skills regarding lethal means reduction counseling and sustained change in beliefs and attitudes about the importance of lethal means restriction following a CALM training. Ensuring that all providers are trained in not only how to assess for the availability of means but also methods of means restriction and empathic counseling to do saves lives.
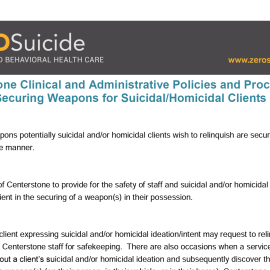
Organization policies should clearly state what clinicians should do regarding lethal means, including the protocol to follow in the event an individual brings a weapon or other lethal means to the clinical setting. Clear policies should be in place for how to document these assessments and actions within the electronic health record (EHR). Centerstone’s Securing Weapons for Suicidal/Homicidal Clients (in the resources section below) serves as a strong example. This protocol outlines the steps for clinical and non-clinical staff to take when an individual brings a lethal instrument to a session.
Questions to consider:
- Are my staff trained in counseling on access to lethal means?
- Are there systems in place to review staff sense of preparedness and support in counseling on access to lethal means?
- What protocols exist for following-up with individuals with access to lethal means?
- What protocols exist for individuals who bring lethal means into our setting?
- What are the local laws on firearm storage?
Discussing lethal means safety should also occur when completing a collaborative safety plan. Please visit the next tab in the Engage section about safety plans for more information.
Suggested Resources
- 1a1bHarvard T.H. Chan School of Public Health. (2016). Means Matter. Retrieved from https://www.hsph.harvard.edu/means-matter/
- 2Hawton, K. (2002). United Kingdom legislation on pack sizes of analgesics: Background, rationale, and effects on suicide and deliberate selfharm. Suicide and Life-Threatening Behavior, 32(3), 223-229. Retrieved fromhttps://onlinelibrary.wiley.com/doi/full/10.1521/suli.32.3.223.22169
- 3a3bLarge, M.M., & Nielssen, O.B. (2010). Suicide in Australia: Meta-Analysis of Rates and Methods of Suicide between 1988 and 2007. Medical Journal of Australia, 192(8), 432-437.
- 4Mercy, J.A., Kresnow, M.J., O’Carroll, P.W., Lee, R.K., Powell, K.E., Potter, L.B., & Bayer, T.L. (2001). Is suicide contagious? A study of the relation between exposure to the suicidal behavior of others and nearly lethal suicide attempts. American Journal of Epidemiology, 154(2), 120-127.
Collaborative Safety Plan
Individualized Approach
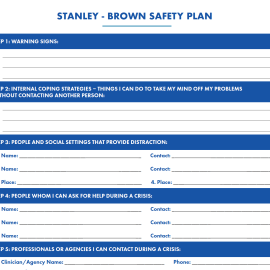
All individuals identified as at risk of suicide should have a safety plan. Collaborative safety planning is becoming a standard in many behavioral health organizations and health systems.
A safety plan is a prioritized written list of coping strategies and sources of support developed by an individual at risk for suicide in collaboration with a clinician. Research shows that individuals with higher-quality safety plans are less likely to be hospitalized in the year after safety planning.1 2Creating unique, customizable safety plans collaboratively rather than presenting a predetermined list of options allows the resource to be tailored to the individual’s needs, comfort, and strengths. It recognizes the individual’s autonomy and expertise on what they find helpful and allows room for adaptations a provider may not have considered.
When creating a safety plan, it is essential that a provider recognize the importance of multicultural humility; what works as a safety measure for one person may not work for another for a multitude of reasons. Providers should enter into the safety planning process with an open mind and sense of curiosity, while also providing knowledge of support measures that have helped others historically.
A safety plan should:
- Be written in the individual’s own words and be easy to read.
- Actively involve the individual’s support systems such as family and friends in the collaborative process, especially to establish their role in responding to times of crisis.
- Be grounded in trauma-informed and recovery orientated approaches, including not assuming families are safe and supportive and that crisis centers are not inherently safe and may lead to police interventions.
- Include counseling on access to lethal means, which is also balanced with respect to legal and ethical requirements under federal and state laws.
- Be revisited and updated regularly and collaboratively during encounters.
- Be in the individual’s possession.
Formats and Protocols
Discussing available formats for the safety plan with the individual allows them to receive a copy in the way in which they are most likely to access it and make use of it. For some, a paper copy may be most useful, while for others, providing information and assistance in accessing electronic or application-based safety planning tools such as the Safety Plan Mobile App or having them take a photo of it to have on their phone would be best.
Regardless of the format the individual chooses, the provider should have a documented copy of the safety plan. Clear protocols should be in place for uploading the safety plan into the electronic health record (EHR), as well as expectations that providers working with individuals for the first time review existing safety plans on file. This helps ensure smooth transitions of care and reduces the need for an individual to repeat themselves. The document should be updated in the EHR each time it is updated with the individual. Organizations should consider having a specific template for the safety plan clearly linked in the individual’s file, ensuring it is easily accessible in times of crisis.
Staff should be trained in creating safety plans, engaging the individual at risk for suicide and any necessary support people, and documenting and following up on the safety plan. It is important to follow up and conduct internal reviews of staff use of safety planning interventions to determine effectiveness, consistent application, and fidelity of this evidence-based practice, and the need for additional staff training or education.
When deciding on the basic structure of the safety plan as well as the clinical process of creating one, the organization should ensure the input of people with lived experience should be centrally incorporated. In addition, receiving feedback from individuals at risk for suicide about their experience with the organization’s safety planning processes should be prioritized as critical perspectives.
Safety planning is not to be confused with contracts for safety or no-suicide contracts. There is no evidence that these contracts are effective; they can increase a sense of stigma and shame for the individual and create a false sense of security for the provider.3, 4 Crisis response planning or safety planning have been found to be more effective than a contract for safety.5 6
Questions to consider:
- What specific safety planning protocols does my organization have?
- How are staff trained in these protocols?
- How are the perspectives of people with lived experience incorporated into this process?
- What local crisis resources can be included?
- How is lethal means safety incorporated into the safety plan?
Suggested Resources
- 1Stanley, B., & Brown, G.K. (2012). Safety planning intervention: a brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256-264.
- 2Stanley, B., Chaudhury, S. R., Chesin, M., Pontoski, K., Bush, A. M., Knox, K. L., & Brown, G. K. (2016). An emergency department intervention and follow-up to reduce suicide risk in the VA: acceptability and effectiveness. Psychiatric Services, 67(6), 680-683
- 3Stanley, B., & Brown, G.K. (2012). Safety planning intervention: a brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256-264.
- 4Rudd, M., Mandrusiak, M., & Joiner, T. (2006). The Case Against No-Suicide Contracts: The Commitment to Treatment Statement as a Practice Alternative. Journal of Clinical Psychology, 62(2), 243-251.
- 5Stanley, B., & Brown, G.K. (2012). Safety planning intervention: a brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256-264.
- 6Bryan, C. J., Mintz, J., Clemans, T. A., Leeson, B., Burch, T. S., Williams, S. R., & Rudd, M. D. (2017). Effect of crisis response planning vs. contracts for safety on suicide risk in U.S. Army Soldiers: A randomized clinical trial. Journal of Affective Disorders, 212, 264-272. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0165032716319474
Next Steps
Engage Patients in a Pathway to Care
The basic next steps to engage individuals at risk are to:
- Establish protocols, templates, and trainings for organizational use of pathways to care, lethal means counseling, and collaborative safety plans with all individuals at risk for suicide
- Engage staff and individuals with lived experience on how best to implement these measures
- Outline timelines for implementation, staff training, and review
- Create templates in the EHR for pathways to care, lethal means counseling, and safety plans.
- Establish protocols to ensure your clinical pathways, templates, and trainings are updated as your implementation progresses as you learn more
- Ensure that instilling hope and actively and collaboratively engaging individuals in their care is as critical as any of the other steps on your pathway to care (e.g., completing a collaborative safety plan and marking it 'done' in the EHR)
Planning Next Steps
There are several additional items to help you plan these next actions:
Quick Guide to Getting Started with Zero Suicide
This one-page tool lists ten actions you can take to start implementation of Zero Suicide.
Getting Further with Zero Suicide
This tool lists several actions you can take if you have been implementing Zero Suicide for a while and are not sure what to do next or need help taking your Zero Suicide work a little further.
Zero Suicide Organizational Self-Study
Every organization should complete the self-study as one of the first steps in adopting a Zero Suicide approach. While the self-study is available in the Lead section of the Zero Suicide online toolkit, it’s provided again here for your convenience.
Zero Suicide Work Plan Template
This form contains an expanded list of action steps to guide your implementation team in creating a full work plan to improve care and service delivery in each of the seven core Zero Suicide components.
Recommendations for Improving Data Collection and Data Definitions
This resource highlights some common questions related to data collection and offers recommendations for improving data collection systems and data definitions. Use this tool to inform discussions about data priorities, data infrastructure needs, and defining quality improvement metrics.