
Boston Children’s Hospital is a participant in the Preventing Youth Suicide Collaborative, a national initiative of leading children’s hospitals committed to advancing the implementation of the Zero Suicide Framework. This important work is made possible through the generous support of the Cardinal Health Foundation, in partnership with the Children’s Hospital Association.
Organization Profile
Boston Children’s Hospital (BCH) is the largest pediatric hospital in New England, with 485 licensed beds, more than 40 clinical departments, and 269 specialized programs. Its Department of Psychiatry offers a full continuum of care, including two inpatient psychiatry units, an acute residential program, a large consultation-liaison service for medical/surgical units, emergency psychiatry in the ED, and several outpatient clinics. BCH also embeds behavioral health clinicians in primary and specialty care settings and operates three primary care practices serving over 27,000 patients. A specialized high-risk service was developed to improve care for youth experiencing behavioral health crises, many of whom present with suicidal thoughts and behaviors.
Implementation of Zero Suicide
In the wake of the pandemic, BCH experienced a sharp rise in pediatric mental health crises. This shift made suicide risk management a top institutional priority and a central quality and safety initiative. In 2020, BCH launched a system-wide quality improvement effort aligned with the Zero Suicide framework and Joint Commission safety goals. The hospital introduced a standardized suicide screening, assessment, and management protocol incorporating:
- Ask Suicide-Screening Questions (ASQ)
- Columbia Suicide Severity Rating Scale (C-SSRS)
- Suicide Assessment Five-step Evaluation and Triage (SAFE-T)
- Stanley-Brown Safety Planning Intervention
More than 600 behavioral health clinicians have since been trained, and compliance with these protocols exceeds 90% across acute services caring for the most severely ill patients.
In 2023, BCH joined fourteen other children’s hospitals in the Preventing Youth Suicide Collaborative, a peer-learning initiative led by EDC. Through this cohort, BCH attended the Zero Suicide Academy, participated in bimonthly Zero Suicide Community of Practice webinars and the annual Zero Suicide workshop. Staff report that the Academy has been energizing and motivating, providing opportunities to share experiences, challenges, and lessons with colleagues from other hospitals. The Academy also validated that BCH was already using many approaches aligned with the Zero Suicide framework and inspired new initiatives, including the inpatient outcomes study and improvements to lethal means counseling processes.
Key Outcomes
Adolescent Psychiatry Outcomes
To evaluate the impact of its Zero Suicide practices, BCH conducted a retrospective study from September 2021 to September 2023 involving 218 adolescents ages 12–17. The study found one of the highest reported rates of prior suicide attempts in this population, underscoring the vulnerability of the group. During hospitalization, patients demonstrated a 54% reduction in suicidal ideation from admission to discharge.
This outcome was achieved by implementing standardized, evidence-based suicide assessment protocols throughout the admission process. These structured assessments anchored care through a suicide-focused lens and informed the use of CBT and DBT sessions, as well as individualized safety planning. Together, these practices helped clinicians provide consistent, evidence-based interventions that supported stabilization.
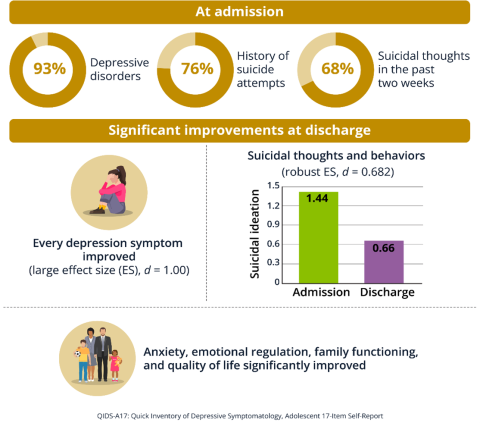
These findings underscore the effectiveness of standardized suicide care protocols.1
Lethal Means Counseling in the Emergency Department
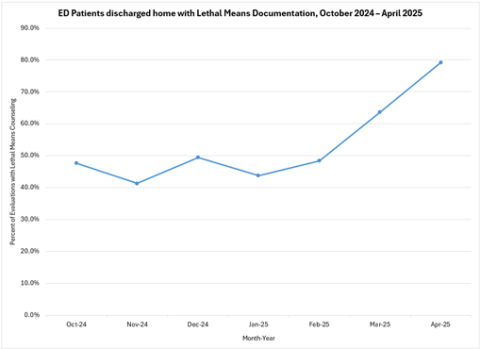
After joining the collaborative in 2023, BCH enhanced its lethal means counseling workflow in the ED. Staff received training through an online course covering suicide risk assessment and management protocols, which included information on lethal means counseling. The process was integrated with the Stanley-Brown Safety Planning Intervention, and families were provided educational handouts such as the American Academy of Child and Adolescent Psychiatry (AACAP) Suicide Safety Precautions at Home. Families have been receptive, with many reporting relief in having clear guidance on making their home environment safer and concrete strategies for supporting their child.
A six-month quality improvement project showed a 66% increase in documented lethal means counseling for patients in crisis discharged from the ED.
Expansion to Primary Care
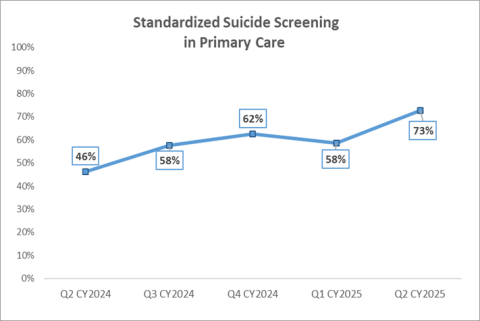
BCH also extended Zero Suicide protocols into its three primary care practices, recognizing that many youth who attempt suicide are seen in primary care before their crisis. Because BCH already had universal mental health screening in place for depression and anxiety during well child visits, the shift was less disruptive for families. Instead, the focus was on building a more robust and standardized suicide assessment and management process for embedded behavioral health clinicians.
Success was driven by two key strategies:
- Engaging key stakeholders from each primary care setting as champions to guide workflows, provide training, and support colleagues
- Regularly sharing suicide screening data with these stakeholders to identify gaps and problem-solve
One challenge was that BCH’s system transitioned to a new Epic EHR during this effort, slowing adoption while staff learned the new system and workflows were migrated. Despite this, utilization of the C-SSRS increased from 46% to 73% within 12 months, demonstrating strong adoption.
Future Steps
Looking ahead, BCH is focusing on the “treat” and “transition” elements of the Zero Suicide framework. To date, 20 multidisciplinary clinicians across psychiatry and primary care have been trained in the Collaborative Assessment and Management of Suicidality (CAMS), with feasibility work underway to expand its use.
Post-discharge, BCH has piloted innovative models to improve continuity of care:
- Inpatient Psychiatry discharge pilot: With support from the Massachusetts Attorney General’s Office, BCH partnered with community providers on an in-home crisis stabilization program. Patients discharged from inpatient psychiatry units received warm handoffs to community programs that provided an average of 148 days of in-home support. Families received sustained follow-up and reported positive experiences, and the lessons learned will inform broader transition strategies.
- ED discharge pilot: BCH’s primary care practices have launched a specialized high-risk service with post-discharge follow-up calls for Medicaid patients seen in the ED for mental health concerns. The goal is to ensure follow-up and care connection within seven days of discharge, helping stabilize patients and prevent readmission.
Through standardized assessments, evidence-based training, enhanced ED workflows, primary care expansion, and innovative pilots, Boston Children’s Hospital has embedded suicide prevention into its culture of care. These efforts demonstrate BCH’s ongoing commitment to protecting youth at risk of suicide and supporting families during their most vulnerable moments.
- 1
The full study can be found in Psychiatric Research and Clinical Practice at the following link: https://doi.org/10.1176/appi.prcp.20240127