Pathway to Care
Continuous Quality Care
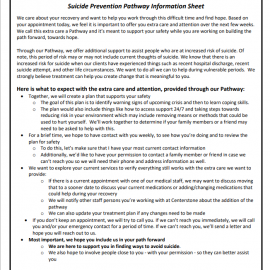
When individuals are at risk for suicide, a pathway to care can be instrumental in working with them to feel safe, secure, and able to stay alive. A pathway to care is a predetermined series of steps to maintain continuous engagement and ensure high-quality care for these individuals. Your organization will need to create a pathway unique to your system, utilizing internal and local resources.
Organizations implementing a pathway to care approach should consider the following to develop your own unique pathway.
In a Zero Suicide approach:
- What services does your organization offer to individuals?
- What referrals or transfers of care will or could happen based on potential progression of risk?
- Who will your organization communicate and coordinate with regarding the individual's care (e.g., primary care, outpatient providers, emergency contacts)? What releases of information and/or MOUs or agreements will be needed to do so?
- How will your organization follow-up with the individual? What contact information is needed to do so?
- How soon after the initial assessment will your organization meet with the individual at risk again?
- What protocols exist within your system if the individual does not come to the follow-up meeting?
- How do staff address lethal means safety with the individual?
- How are the voices of people with lived experience being incorporated into the development of your suicide care pathway?
Outlining a Pathway
An effective pathway to care creates a sense of direction for both the individual at risk and the provider. It can help a provider remain clear and steady during a suicide evaluation and increase the trust the individual has in the system’s competence and compassion. As such, it is important that each organization’s pathway to care is clearly and carefully outlined for both staff and the individuals they serve.
Clear documentation should be provided to anyone on a pathway to care explaining what it is, what they can expect, and who they can contact. Evidence shows that individuals at high risk of suicide are often among the highest percentage of those who drop out of treatment; a clearly established pathway can increase the likelihood of the individual remaining engaged.1
Assuring all staff are not only informed of pathways to care but properly trained in their use is a necessary step for proper implementation. Organizations should provide initial trainings in pathways for staff members, as well as hold regularly scheduled refresher trainings. Measures should be in place to ensure providers feel confident and capable to use a pathway to care effectively.
Electronic Health Record
Processes for documenting the established pathway to care and takeaways from the conversation with the individual into an electronic health record (EHR) should be clearly laid out for staff.
Further, staff beginning work with an individual they have not worked with previously should become familiar with reviewing charts within the EHR for information on their pathway to care. Promoting consistent and effective use of an EHR promotes a uniform treatment plan and reduces an individual’s need to repeat themselves.
Lived Experience
As is true for all elements of the Zero Suicide framework, it is imperative that voices of lived experience are involved in the creation and implementation of the pathway to care. People who have experienced suicidality should be actively engaged in creating what the pathway includes, what language is used, how staff are trained, and how to engage with individuals. As the organization implements and periodically reviews its use of the pathway to care, people with lived experience should be at the center of the conversation throughout. Similarly, as part of active engagement, as individuals at risk for suicide find increased stability, their input on the pathway to care based on their own reactions and perceptions should be incorporated.
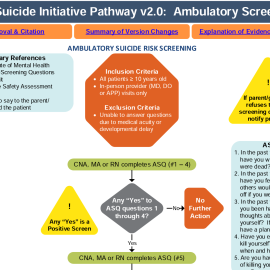
Active Engagement for Safer Suicide Care
A fundamental premise of the Zero Suicide approach is that safer suicide care begins from the moment the patient calls the organization for an appointment or is admitted for treatment. For example, suicide risk immediately becomes a primary focus of assessment in a behavioral health or primary care setting if a patient indicates that he or she is currently having suicidal thoughts, has had suicidal thoughts in the past, or has made prior attempts.
Another fundamental premise is that all staff members have a crucial role in preventing suicide. Suicide risk should be assessed collaboratively, compassionately, and frequently with patients who are at risk of suicide. The frequency of assessment may depend on a number of factors specific to your organization and patient populations, however, all providers should be aware and prepared to collaborate with the patient around their suicide risk. This attention to individuals at risk for suicide by all staff members, clinical and non-clinical, requires a fundamental shift in what a health or behavioral health organization sees as its role.
Although a great deal of the focus of Zero Suicide is keeping patients safe from harm, engaging patients is not solely about making sure that they come in for visits. The goal is for patients to grow, gain skills, and recover. The patient and provider relationship and rapport plays a major role in the disclosure of suicide risk by the patient and their subsequent engagement in their care. Care that is compassionate, empowering, and strengths-based builds on the trust between provider and patient can help to support the patient on their path to recovery. Further, care does not begin and end only within the time spent with the patient face-to-face in care, but also involves contact between visits when needed, as well as during transitions in care.
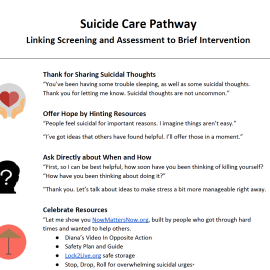
Actively engaging a patient about suicide risk:
- Takes into account the individual’s experiences and resources and gives them a voice in their care
- Builds hope for recovery
- Empowers the individual to resolve crises and long-term problems using the least invasive methods possible
The result of active engagement in suicide care is that the patient feels heard, cared for, and empowered to make safe decisions.
Care that focuses on suicidal thoughts and behavior may be new and even overwhelming to a patient and family. The collaborative, nonjudgmental, comprehensive approach that is part of Zero Suicide may be a very different experience for many patients with suicide risk, especially if prior treatment has failed them. Staff members will need to take care to let patients know what to expect and guide them in how to use treatment effectively.
As you are planning your implementation of the Engage element, consulting with your implementation team members with lived experience regarding the best ways to do this will allow your organization to implement guidelines and standard care practices that meet the goals set forth within this element.
Caring Contacts as Non-Demand Engagement
One evidence-based way to supportively engage individuals is the use of non-demand caring contacts. These contacts are brief communications that are non-demand (meaning they don't ask the individual to do something) and show support. Research has found that this low-cost and scalable intervention can have significant effects on an individual. Not only can they promote connection to care and increase their participation in collaborative treatment, caring contacts have also been shown to decrease reports of suicidal ideation and suicide attempts compared to the standard of care in a wide variety of health and behavioral healthcare settings.2, 3, 4
The use of caring contacts can help engage and re-engage individuals in care when they miss appointments, choose to stop treatment, and during care transitions or discharge from care. They may be especially helpful to individuals who have barriers to care or are unable or uninterested in accessing treatment.
As part of your care pathway for individuals at higher risk of suicide, it's critical to consider the populations you serve, the channels through which individuals prefer to receive communication (texts, letters, emails, care portal messages) and the content of the messages.5 For more information about caring contacts and examples of caring contacts from a variety of systems, visit the Transition element.
Suggested Resources
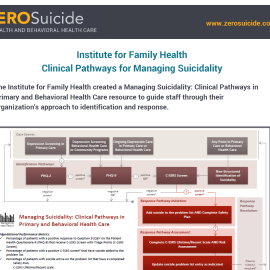
Care Pathway Resources
Sample Care Pathways
Other examples of care pathways are available in the resources section.
- 1Stanley, B., and Brown, G.K. 2012. Safety planning intervention: A brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256-264.
- 2Comtois KA, Kerbrat AH, DeCou CR, et al. Effect of Augmenting Standard Care for Military Personnel With Brief Caring Text Messages for Suicide Prevention: A Randomized Clinical Trial. JAMA Psychiatry. February 2019.
- 3Luxton, D. D., June, J. D., & Comtois, K. A. (2013). Can postdischarge follow-up contacts prevent suicide and suicidal behavior? A review of the evidence. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 34(1), 32.
- 4Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52(6):828-833.
- 5Reger, M. A., Luxton, D. D., Tucker, R. P., Comtois, K. A., Keen, A. D., Landes, S. J., Matarazzo, B. B., & Thompson, C. (2017). Implementation methods for the caring contacts suicide prevention intervention. Professional Psychology: Research and Practice, 48(5), 369–377.