Risk Formulation
Forming a Clinical Judgment of Risk
Clinicians are often faced with having to make judgment calls about suicide risk with insufficient or contradictory information. Information obtained in a suicide screen is just one part of what is needed to fully assess risk and develop the best care plans to engage clients. Establishing a collaborative and shared perspective is essential to obtaining a comprehensive understanding of the client’s suffering and strengths.
One prevalent method of assessment attempts to put people into predictive categories such as low, medium, or high risk. Despite many efforts to define these terms, definitions were usually difficult to apply, and the terms lack predictive validity, cross-clinician consistency, and clinical utility in treatment planning.1
The high-medium-low model of formulating risk also was not anchored in a context. One could ask, “high compared to what?” or “low compared to when?” In newer, contextual risk formulation methods, the primary purpose is planning rather than prediction of suicide.1
Risk Formulation Model
The model pictured below draws from prevention research and advances in violence assessment.2 While the figure from Assessing and Managing Suicide Risk (AMSR) shows just one way of organizing a risk formulation, the goal is to develop a personalized plan for each individual that is anchored in the clinical or community setting and in the individual’s own history over time. The clinical judgment about risk, combined with the entire formulation, can help with decision-making about what intervention or treatment setting the person needs.
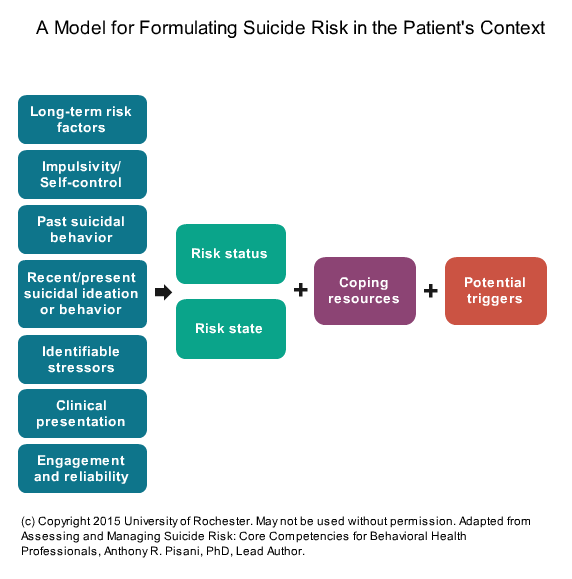
The column at the left in the diagram shows the key information needed to support a risk formulation.
Risk status, risk state, coping resources, and potential triggers comprise the “risk formulation” in this model.
A well-documented risk formulation can demonstrate that clinical decisions were sound and aid in communication with the client, other clinical staff, and important people in the client’s life. Clear documentation also helps to show the rationale behind your formulation, discussions with the client about your risk formulation, and treatment decisions. As new information becomes available and circumstances change, the assessment of risk also should be reconsidered and possibly modified. Clear documentation of risk and the rationale for treatment recommendations will provide a better defense against legal challenges than poor or incomplete documentation.
This interactive is best experienced on desktop browsers and may not work on all mobile devices.
- 1a1bPisani, A. R., Murrie, D. C., & Silverman, M. M. (2016). Reformulating suicide risk formulation: From prediction to prevention. Academic Psychiatry 40(4), 623–629. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/26667005
- 2Douglas, K. S., & Skeem, J. L. (2005) Violence risk assessment: Getting specific about being dynamic. Psychology, Public Policy, and Law, 11(3), 347–383. Retrieved from http://dx.doi.org/10.1037/1076-8971.11.3.347
