
The Ridge Behavioral Health System, located in the heart of Bluegrass Country, provides a variety of behavioral health services to people throughout the state of Kentucky. Owned and operated by Universal Health Services (UHS), the largest facility-based behavioral health provider in the United States, The Ridge was tasked with transforming suicide care by partnering with the Zero Suicide Institute. In alignment with Zero Suicide framework elements, The Ridge focused on suicide assessment, risk formulation, and ongoing management of suicide risk.
Key Outcomes:
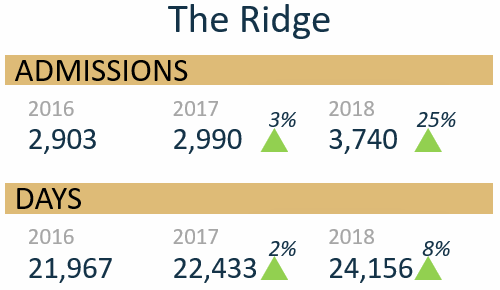
- One year after implementation of Zero Suicide, our enhanced protocol and uniformity increased reliability in risk assessments and risk formulations resulting in a 25% increase in the number of inpatient admissions to the facility and an increase of 8% in the total number of patient days.
- Patient satisfaction on two key questions at discharge, “I felt safe while I was there” and “I feel better now than when I was admitted,” showed significant improvement.
About The Ridge Behavioral Health
Located in Lexington, Kentucky, The Ridge is accredited by the Joint Commission as a licensed, 110-bed hospital. Inpatient care is provided on a 24-hour basis, seven days a week. Outpatient and partial hospitalization services are provided on a five-day per week basis, during the days and evenings. The Ridge offers a healing environment, providing mental health and substance use disorder services to children, adolescents, adults, and older adults.
Getting Staff Engaged with the Zero Suicide Initiative
The selection of The Ridge to participate in the Zero Suicide initiative honored and excited our CEO, who eagerly shared the news with the Senior Leadership Team. The first step the CEO took to promote this initiative was to identify an enthusiastic and passionate champion/cheerleader. The champion secured the CEO’s support to create a formal, multidisciplinary implementation team, which included the CEO, the Director of Performance Improvement, Director of Risk Management, Chief Clinical Officer, one intake supervisor, one nurse manager, one staff nurse, one mental health technician, and one therapist. To ensure those selected knew this was an honor and to secure their acceptance, each received an email congratulating them on being selected and providing a brief overview of the project. Happily, no one declined the invitation.
The Ridge announced the Zero Suicide initiative to all staff via an email from the CEO, who framed the initiative as an honor bestowed upon The Ridge to be chosen to participate. The email outlined the meaning of Zero Suicide and the connection to The Ridge’s mission to provide superior quality patient care. Verbal communication was delivered throughout the facility to groups such as the Medical Executive Committee, management team, and unit/departmental staff meetings. Posters regarding the launch of the initiative and other printed educational materials were placed throughout the facility in areas frequently visited by staff, such as at the time clocks and in break rooms.
The Zero Suicide Implementation team attended the Zero Suicide Virtual Academy between October 20 and November 9, 2016, and they participated in the online community of practice from December 2016 through June 2017. The team also completed the Zero Suicide Organizational Self-Study.
The Ridge Enhancements to Suicide Assessment Process and Environment of Care
Suicide Risk Assessment
Content from the Virtual Academy and results from the Zero Suicide Organizational Self-Study helped the team to focus their actions. Policies and procedures related to suicide risk, assessment of patients, patient observations and rounding, and high-risk behavior precautions were reviewed and revised to reflect elements in the Zero Suicide framework. One action taken was to replace our existing training on suicide risk assessment with a formalized suicide risk assessment tool. The Ridge, along with other UHS facilities, chose Assessing and Managing Suicide Risk (AMSR), which includes suicide assessment, risk formulation, and ongoing management, as our new evidence-informed training.
In an effort to tie Zero Suicide to AMSR, two Zero Suicide implementation team members were selected to become AMSR trainers. As their first assignment, these AMSR trainers were tasked with training the implementation team in late 2016 and early 2017, followed by all registered nurses, therapists, and intake staff. The training was, and still is, used as a platform to discuss our involvement with the Zero Suicide initiative. Once clinical staff were equipped with knowledge and resources, our next step was to replace the existing tools for suicide assessment in intake and the daily reassessments conducted by nursing with evidence-informed AMSR assessment tools.
The Ridge Intake and Assessment Department made important revisions to our processes at the front door. Once patients enter through the front door, our receptionists started conducting 15-minute observation checks and took a photograph of the patient for identification purposes. Prior to the Zero Suicide initiative, all patients admitted to inpatient services worked with their treatment team throughout their stay to develop a crisis safety plan that was finalized at discharge. Additionally, all patients admitted to outpatient services and partial hospital programs (PHP) worked with a health care professional to develop a crisis safety plan at the time of admission and again at discharge. Our current practice is an enhanced Crisis Safety Planning process through which anyone assessed by the Intake Department who does not meet admission criteria develops a crisis safety plan with an intake counselor prior to exiting the facility. The plan includes the following:
- Three referrals
- The Ridge’s phone number
- The National Suicide Prevention Lifeline phone number and website
- Lists of triggers, warning signs, and coping strategies
Check here to download the complete crisis safety plan.
Environment of Care
One of the key factors in the Safety Planning Intervention is making the environment safe. In 2017, modifications were made to the existing environment of care (EOC) assessment tool to address safety and ligature risks throughout the facility. Identified suicide risks were assessed and mitigation plans were established and prioritized. The modified assessment tool was shared with all UHS behavioral health facilities. We have made numerous environmental improvements since 2017 to reduce the risks of suicide in the facility, such as ligature-resistant doorknobs, showerheads, sinks, toilets, and furniture. Environmental rounds are ongoing, and both findings and improvements are shared with staff on a regular basis through the intranet, staff meetings, town hall meetings, and postings throughout the facility.
Practices related to patient safety checks were also revised. An element of the Safety Planning Intervention is recognition of signs that immediately precede a suicidal crisis. Patient observation is seen as a prevention opportunity to continuously look for changes in behavior, including the presence of risk factors. We now engage patients who enter the front door by informing them of the safety checks. We let them know that their safety is our number one priority. At least every 15 minutes, staff will go around to check on them and tell them that this is their opportunity to let us know if anything has changed. The patient handbook was revised to include specific information about safety checks and how they will occur around the clock.
“To assess the impact of our Zero Suicide implementation efforts, the following were analyzed from 2016 to 2018: data on admissions, total number of days that patients spent in the hospital, and patient satisfaction.”
Our Philosophy of Care
We asked ourselves how we as a hospital could incorporate the lived experiences of suicide attempt and loss survivors into our practice. We collaborated with the National Alliance on Mental Illness (NAMI) to identify survivors of suicide loss, including family members of a person who died by suicide who were willing to share their experiences with The Ridge employees. The experiences these survivors shared with staff about how they found hope and recovery have been embedded into our staff trainings. We also have NAMI representatives lead a weekly group on our inpatient adult psychiatric unit, during which they share their lived experiences with suicide.
Our involvement in the Zero Suicide initiative made such an impact on our philosophy of care that we wanted to share our insights and philosophy with the community. In 2018, The Ridge hosted 350+ attendees at the Suicide Across All Ages and Stages Conference, with keynote speaker Kristen Quinlan, PhD, of the Suicide Prevention Resource Center at Education Development Center.
The Ridge Data and Outcomes
To assess the impact of our Zero Suicide implementation efforts, the following were analyzed from 2016 to 2018:
- Data on admissions
- Total number of days that patients spent in the hospital
- Patient satisfaction
Data indicate that implementing the safer suicide care components of the Zero Suicide framework, specifically our improved discharge planning process and formalized staff training on suicide risk assessment, in combination with our crisis safety planning efforts, have led to increased admissions, increased number of inpatient days in treatment, and increased patient satisfaction.
Our baseline number of admissions in 2016 was 2,903. During year 1 after Zero Suicide implementation and the first phase of AMSR training, we saw a 3% increase in admissions to 2,990. In year 2, 2018, we admitted 3,740 patients, a jump of 25% in admissions. The number of inpatient treatment days increased 2% in 2017 and another 8% in 2018. It is possible that admissions and the number of inpatient days in treatment increased due to our enhanced protocol and uniformity, which increased reliability in risk assessments and risk formulations. Similar to the ED-SAFE study—when they implemented universal screening for suicide risk—the detection rate doubled (i.e., they found more patients who had a past attempt or current ideation).
Satisfaction surveys are provided to all of our inpatients at the time of discharge. Patients are able to complete these confidentially or with staff assistance. The responses are scored on a scale with (5) Strongly Agree, (4) Agree, (3) Neutral, (2) Disagree, and (1) Strongly Disagree. The annual response rate for 2016 to 2018 ranges between 78% and 92%. On the question, “I felt safe while I was there,” the mean score in 2017 was 4.51, and it increased in 2018 to 4.57. On the question, “I feel better now than when I was admitted,” the 2017 mean score was 4.62, and it jumped to 4.72 in 2018.
The Ridge: Next Steps
To continue to improve care related to our key outcomes, The Ridge will keep the Zero Suicide implementation team active. New members were selected in 2019, and they began the Zero Suicide Virtual Academy in June 2019. While staff support the idea of zero suicides, the language associated with AMSR (risk state and risk status) is hard for the staff to grasp. To address this, we plan to engage the medical staff early on to increase staff awareness and use of the language.
Going forward, we also plan to enhance physician buy-in with additional training in suicide prevention. All of our licensed therapists received AMSR retraining beginning in May 2019. AMSR training helped prepare our staff for our July implementation of day-of-discharge suicide risk assessments done by licensed therapists. This assessment is completed in addition to the daily assessment by a registered nurse and the discharge assessment by the physician.
To enhance patient observations, The Ridge added electronic tablets to record observation rounding on our patients. The new tablets identify patients with a color photograph, name, level of observations, high-risk precautions, and the last two results of safety checks. They also prompt staff when a round is needed by changing the image’s color. This visual cue alerts staff and improves timeliness of observation rounding. We would also like to extend our partnership with NAMI to include in-person representatives to add the lived experience perspective to new employee orientation. Lastly, The Ridge is considering the addition of caring calls (at least for a higher-risk population) and caring cards for discharged patients.
Authorship Details
- Kellie Holland, MSN, RN, Chief Operating Officer/Chief Nursing Officer, The Ridge Behavioral Health System
For more information, email Kellie.Holland@UHSInc.com.