
Riveredge Hospital is the largest free-standing psychiatric facility in the state of Illinois and is part of the Universal Health Services (UHS) system which is the largest inpatient psychiatric hospital system in the United States. Since 2015 dozens of hospitals across the UHS system have implemented Zero Suicide. Riveredge started implementation of Zero Suicide in 2016 with a focus on care transitions as a key priority. This included implementing a “Bridge Appointment” that ensures patients meet with a clinician as part of the discharge planning process.
Key Outcomes:
- As of mid-2018, 90% of all patients being discharged from inpatient treatment received a “Bridge Appointment.”
- In 2017 there was a 21% decrease in the 30-day readmission rate compared to the previous year.
About Riveredge Hospital
Riveredge Hospital is the largest free-standing psychiatric facility in the state of Illinois. Located just west of the city of Chicago, we are licensed for 210 inpatient beds. We treat children, adolescents and adults inpatient as well as have the only unit for adults with intellectual disabilities in the state. Riveredge Hospital also offers treatment across the continuum including partial hospitalization, intensive outpatient and traditional outpatient treatment.
Riveredge Hospital Enhanced Discharge Process
In our continuing journey to provide quality comprehensive mental health services across the continuum of care, Riveredge Hospital began implementing the Zero Suicide framework in the fall of 2016. During the initial phase of this initiative, the executive leadership team completed the Zero Suicide Organizational Self Study. Additionally, the Zero Suicide Workforce Survey was administered to all hospital staff. The survey focused on identifying how prepared staff felt in providing care to suicidal patients. Hospital leadership discovered a lack of comfort from staff in directly asking patients about suicide. The Zero Suicide Workforce Survey results helped our leadership team identify staff training and resource needs. These identified needs included increased training on suicide prevention and awareness, suicide screening practices, and how to communicate with patients about suicide.
In order to meet the need for additional suicide prevention training, the next step of Zero Suicide implementation involved the leadership, clinical, and non-clinical staff completing the Assessing and Managing Suicide Risk Training (AMSR). The AMSR curriculum teaches care practices recommended by the nation’s leading experts in the research and delivery of suicide care. Implementation of Zero Suicide at Riveredge is guided by the AMSR training as reflected by revising initial and ongoing risk assessment processes, enhancing communication between teams, and increased involvement from the patient’s support system. To reflect these revised assessment processes, the hospital made changes to several hospital forms of documentation including the initial intake assessment, the Daily Nursing Note and Assessment, and the discharge safety plan. AMSR language including risk status/risk state, documentation of interventions to mitigate suicide risk and the Columbia Rating scales were added to multidisciplinary forms. Some of the hospital staff became certified AMSR trainers, and they trained clinical staff on how to use the new documentation by showing them examples of completed updated forms. Additionally, the discharge practices outlined in the AMSR training highlighted how critical care transitions are for patients at risk for suicide, and inspired us to improve our discharge process to help transition our patients back to the community and to reduce the risk of patient readmissions and suicide attempts.
The Bridge Appointment
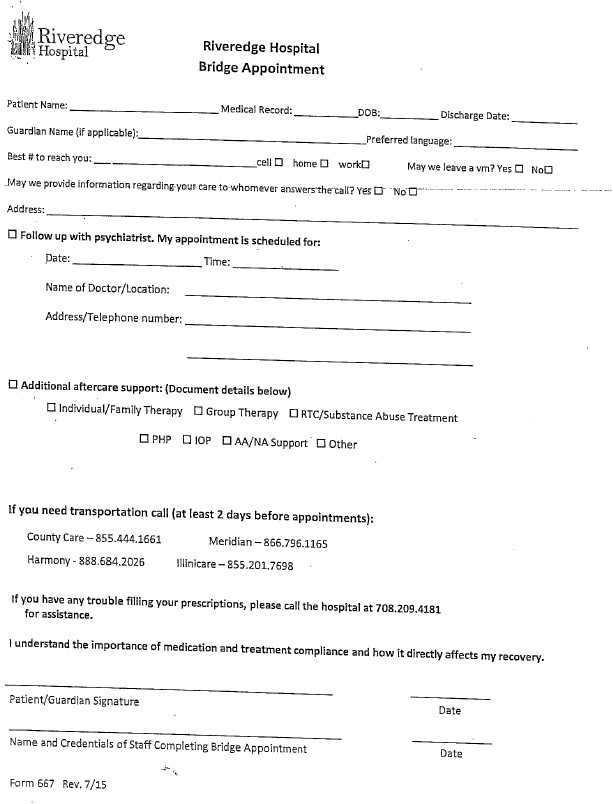
We continued to implement Zero Suicide and focused on the “Transition” element of the Zero Suicide Toolkit. To further improve care transition processes, we created a new workflow step where all patients come down to our admissions department to meet with another clinician as the final step in their discharge process. The purpose of this step, called a “Bridge Appointment,” is to review the aftercare plan including appointments, medications, and any transportation concerns to attend these appointments. The clinician also reviews the discharge safety plan one last time with both the patient and their identified support person. This provides the opportunity for the patient and their support system to review the plan together, ask additional questions, and review any potential obstacles in adhering to the established plan. As of 2nd quarter 2018, Bridge Appointments were completed for 90% of all patients being discharged from inpatient treatment, excluding those transitioning to another 24-hour setting.
The purpose of…a “Bridge Appointment,” is to review the aftercare plan including appointments, medications, and any transportation concerns to attend these appointments. The clinician also reviews the discharge safety plan one last time with both the patient and their identified support person.
A Bridge Appointment form was created and is utilized for documenting a patient’s aftercare in a more patient-friendly format. In addition to the aftercare appointments, the form includes transportation resources and a review of the importance of taking medication as prescribed. Patients are encouraged to contact the facility if there are any difficulties in filling prescriptions that may occur due to insurance issues.
Following implementation of Bridge Appointments hospital-wide in January 2017, a decrease in 30-day readmission rate was noted from calendar year 2016. The completion of Bridge appointments had a positive impact on the patient and family experience and facilitating transition to the next level of care.
30-Day Readmission Rates:
| Period | % of change from previous year |
|---|---|
| Prior to implementation of Zero Suicide initiatives | |
| 2016 | 7% increase |
| Following implementation of Zero Suicide initiatives | |
| 2017 | 21% decrease |
| 1Q – 2Q 2018 | 13% decrease |
Figure 1. Bridge Appointment Form (click to enlarge)
Discharge caring calls
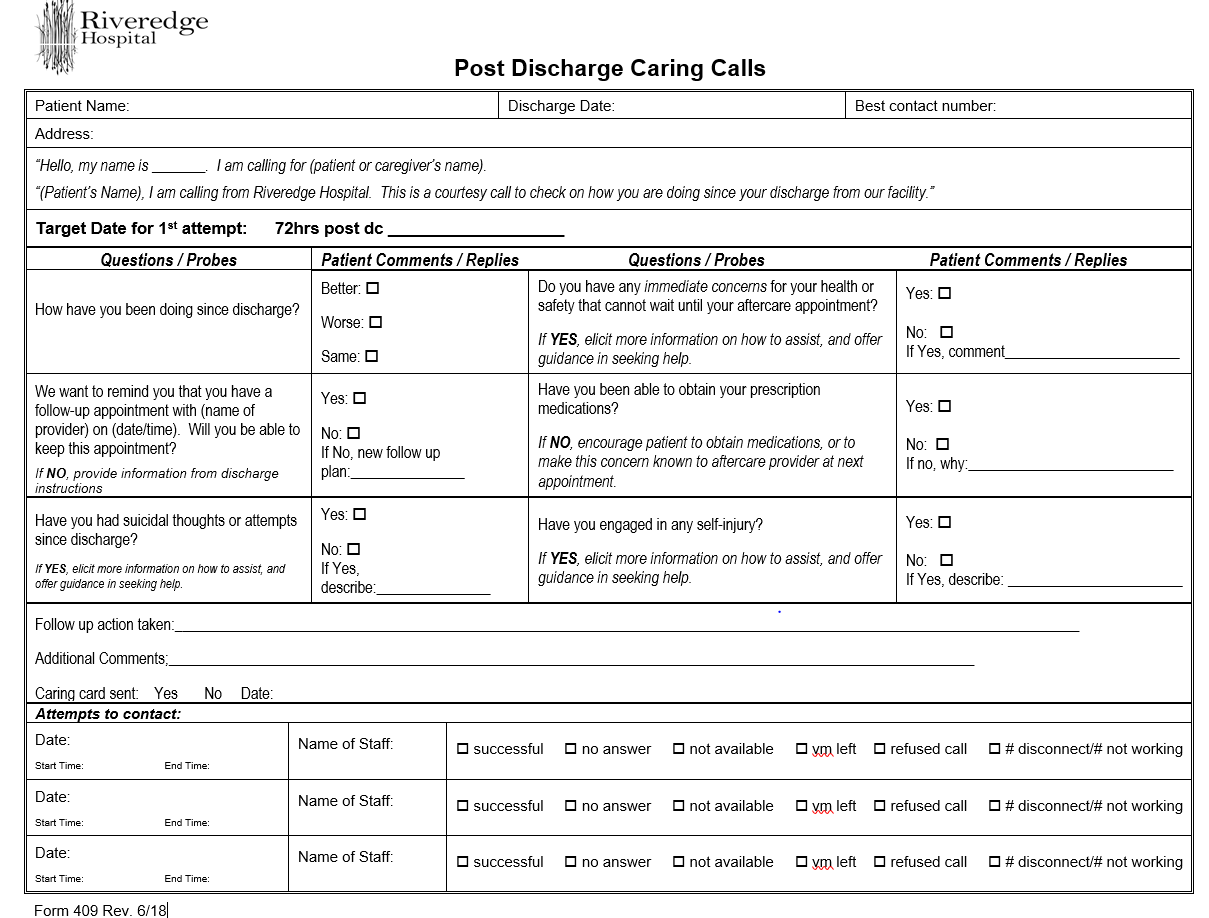
Due to the success of the Bridge appointments in reducing readmissions, our leadership identified an additional opportunity to improve patient outcomes and reduce readmissions by implementing post-discharge caring calls within 72 hours of hospital discharge. This initiative was piloted on the hospital’s inpatient adult units 4th quarter of 2017 and then expanded hospital-wide January 2018. Highlights of the post-discharge caring calls protocol include the following:
- Discharged patients are contacted within 72 hours of discharge.
- Three attempts are made to connect with the patient.
- The clinician completing the post-discharge caring calls reads from a script (see figure 1 below) to assess level of functioning, any immediate concerns for health or safety, and again reviews the follow-up appointments and ability to keep the appointment.
- The clinician assess the patients/family’s ability to obtain their prescriptions.
- Referrals are made as needed.
- The hospital staff offers assistance in rescheduling appointments, coordinating transportation, and troubleshooting difficulties in filling prescriptions.
These calls have allowed the hospital team to provide support to patients and their support system during their recovery. For example, in one of our post-discharge caring calls it was identified that an adolescent patient was at risk for readmission since her discharge 48 hours prior and return to school. During her Bridge appointment, the patient and family chose not to attend the partial day program after inpatient discharge due to the adolescent wanting to return to school. When the caring call was made, our staff recommended that the family bring the adolescent back in for an assessment. We were able to start the adolescent in our partial day program the next day. She successfully completed that program and transitioned back to school, avoiding readmission.
Another example occurred when an adult patient disclosed that they had misplaced their aftercare plan and paperwork during their caring call. The information gathered on the Bridge Appointment form assisted staff in providing the aftercare information to the patient, including the date and time of appointment and contact information.
Caring call completion is audited monthly, and strategies to improve successful contact with patients implemented. As of 2nd quarter 2018, 61% of patients were reached to complete the caring call. The percentage of calls completed or attempted has also improved with the 94% compliance reported for 2nd quarter 2018. If a patient has not been reached via telephone, the staff sends a Caring Card via mail to their address given during the Bridge Appointment. The Caring Card encourages them to call us with any concerns they are having, and serves as a reminder that we care about their recovery.
Figure 2. Post Discharge Caring Calls Script (click to enlarge)
Future plans for Zero Suicide Implementation
As a next step of our Zero Suicide initiative, we plan to address trends related to medication adherence that have been identified through our post-discharge caring calls. In addition to insurance issues related to medications, patients and family members report not filling their prescriptions at the time of the call. Hospital staff are working to identify a community partner to assist with insurance issues and filing prescriptions prior to discharge from the facility or delivering to their home.
In addition to the enhanced discharge process, Riveredge Hospital continues to focus on more intensive training related to patients risk state and risk status, as well as the development of additional tools to assist staff in creating individualized suicide care plans for their patients. We plan to redistribute the Zero Suicide Workforce Survey during the third quarter of our fiscal year to identify staff training and resource needs.
Authorship Details
- Carrie Overbey, LCPC, Chief Clinical Officer
- Carol Carlson, RN, Director of Performance Improvement
- Sarah Martinez, LCSW, Coordinator of Assessment and referral
For more information contact Carrie Overbey at 708-209-4169.