The Mental Health Center of Greater Manchester (MHCGM) in New Hampshire is a private, nonprofit, Certified Community Behavioral Health Clinic (CCBHC). With its mission of transforming the lives of individuals, families, and the community, MHCGM has provided an evidence-based, comprehensive system of behavioral health care to the Greater Manchester community for nearly 65 years.
The following Zero Suicide Outcome Story is an update to the Mental Health Center of Greater Manchester Outcome Story first shared in January 2020. This update captures subsequent developments and impacts through 2024.
Since implementation of the Zero Suicide approach, MHCGM has accomplished the following:
- Decreased suicide deaths by an average of 33% compared with the 8 years prior.
- Trained 94% of staff in suicide prevention.
- Assessed suicide risk in 93% of active clients in 2024.
Organizational Profile
Designated as a CCBHC by the NH Bureau of Mental Health Services, MHCGM annually provides a broad range of services to nearly 10,000 individuals, including adults, children, seniors, and veterans. The largest provider of outpatient behavioral health services in New Hampshire, MHCGM has over 450 employees operating over 30 programs and is affiliated with the Geisel School of Medicine at Dartmouth. MHCGM is located in downtown Manchester, which constitutes New Hampshire’s urban center, and is a federal refugee resettlement zone. The population of Manchester is 77% White, 13.4% Hispanic, 4.6% Asian, 5.3% Black/African American, and 10% two or more races.
Within our continuum of projects, programs, and initiatives, MHCGM provides evidence-based recovery and resiliency services throughout our inpatient, outpatient, community/home/ school-based and residential programs. These include services such as:
- Child, Adolescent, Adult and Older Adult services
- Assertive Community Treatment
- Crisis Response Services
- Crisis Stabilization Services
- Acute Residential Treatment Program.
- Homeless Outreach Services
- InSHAPE Healthy Choices/Healthy Changes program
- ProHealth Integrated Care program
- Medication Services
- Vocational Services
- Supportive Housing Services
- Care Transition Services
- Substance Use Disorder services
- Medication Assisted Recovery (MAR)
- Transcranial Magnetic Stimulation (TMS)
- Research studies
Implementation of the Zero Suicide Framework
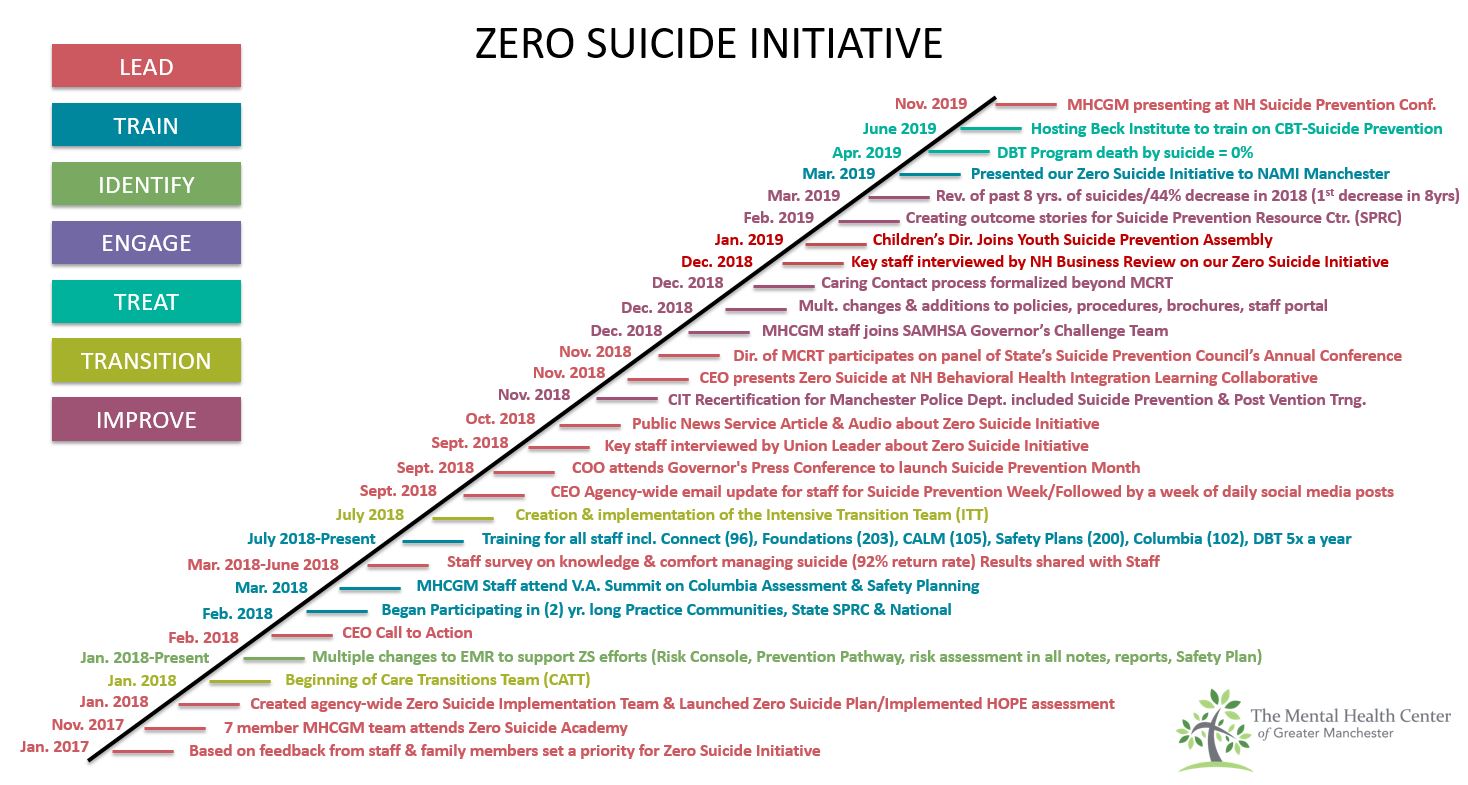
In early 2017, MHCGM set the implementation of the Zero Suicide framework as a priority based on feedback from agency staff and family members of patients. Later that year, seven MHCGM team members attended the Zero Suicide Academy, which prompted the creation of an agency-wide Zero Suicide Implementation Team in January of 2018.
Also in 2018, the team began to implement our Zero Suicide Plan, and our president and CEO formally announced a call to action. From there, MHCGM’s Zero Implementation Team began to discuss and implement specific steps pertaining to the seven elements of the initiative: Lead, Train, Identify, Engage, Treat, Transition, and Improve.
See early timeline below. Click here for the full timeline.
Figure 1. MHCGM Zero Suicide Initiative Timeline
To date, a variety of key MHCGM staff and partners have attended four additional Zero Suicide Academies and have broadened the membership of the implementation to include individuals with lived experience, Director of Data Science, Zero Suicide Grant Project Director, Director of Training and Staff Development, Medical Staff leaders, and specialized population liaisons such as those working with veterans. In 2022 MHCGM experienced a transition in CEO and continued to sustain a high-level of Senior Leader support and engagement with our Zero Suicide initiative with our former COO and co-leader of our Zero Suicide Implementation team becoming our new President and CEO.
As the timeline suggests, changes to our organization have occurred at every level, from administrative protocols to service delivery. In an effort to ensure agency-wide implementation, position-appropriate trainings are required of all staff. We currently offer 13 different suicide prevention-related trainings (see training section for more detail).
These trainings have resulted in increased awareness of risk factors, protective factors and warning signs, which inform personal interactions with patients, families, and community members. Analysis of the most recent Zero Suicide Workforce Survey conducted by our center in 2023 found that 94% of staff have received training regarding the warning signs for suicide, compared to only 65% in 2018. In addition, 90% percent of staff responsible for treatment of patients on the suicide risk pathway feel confident being able treat them as well.
Implementation of Zero Suicide in Health Systems Grant
In 2021, MHCGM received a 5-year grant from SAMHSA to expand our Zero Suicide efforts to include community partners. MHCGM partnered with The Manchester Veterans Administration (VA) and Catholic Medical Center’s Healthcare for the Homeless Program (HCH) to create a suicide-safer system of care through the implementation of the Zero Suicide framework. MHCGM has spearheaded this collaboration with the VA and HCH to establish a leadership-led culture of suicide prevention across all partner organizations. A key component of this initiative is training staff in evidence-based practices to ensure at-risk individuals receive care that meets their unique needs. The partnership has focused on multiple elements of the Zero Suicide framework over the course of the grant, including building organizational leadership devoted to championing Zero Suicide implementation, identifying those at risk of suicide, engaging individuals into services, and extensive training of staff in evidence-based suicide prevention.
As part of the grant initiative, three coalitions were also developed to focus on special populations at high risk of suicide. These include Service Members Veterans and Families (SMVF), those experiencing homelessness, and older adults. The coalition leaders work with community partners to identify the needs and risk factors associated with these groups and to ensure they receive needed services. These community partners include the New Hampshire Suicide Prevention Council Subcommittee for SMVF, Manchester Continuum of Care, and NH Care Path, among others.
Enhancements to our System of Care
Our electronic medical record (EMR) system has been enhanced to now include a patient suicide risk console viewable to all patient-facing staff, which allows universal awareness of suicide risk, appropriate interventions, and planning to prevent death by suicide. Additionally, policies and procedures have been implemented regarding care transitions to ensure warm hand-offs. Caring contacts are now a standard part of care within our crisis care programs and throughout the organization.
Our Mobile Crisis/ Rapid Response team often deploys with the Manchester Police Department (MPD) to help diffuse crises in the community. As part of this initiative, MHCGM provides MPD officers with Crisis Intervention Training (CIT) to effectively and compassionately assist those in need.
Once a level of suicide risk and condition is identified, whether chronic or acute, appropriate intervention is initiated per the Risk Stratification Table provided by the US Department of Veterans Affairs Rocky Mountain MIRECC for Suicide Prevention. Reassessment, safety planning, caring contacts, assignment to the Suicide Risk Care Pathway, and follow-up appointments are planned by the clinician as indicated.
“At MHCGM, we believe that suicide prevention is everyone’s responsibility. It is both our duty and our mission to foster hope and embed the principles of Zero Suicide into the very fabric of our community healthcare system—working relentlessly to reduce suicide deaths among those we serve.”
Patricia Carty, President and CEO of The Mental Health Center of Greater Manchester
Screening
Because MHCGM provides various levels of care at multiple locations via office-based and community-based teams, suicide risk is identified and assessed through screening, assessing, and risk formulation early and often. We use the Patient Health Questionnaire (PHQ-9/A) universally upon intake and at each prescriber visit.
We also use the Columbia Suicide Severity Rating Scale (C-SSRS) at any visit where risk is identified, as well as for the following:
- All Rapid Response (Crisis team) visits/deployments in the Emergency Department, office, and community.
- All emergency services visits and Emergency Department discharges to home after extended stay (C-SSRS Discharge Screener version)
- At the Cypress Center Inpatient Unit during stay and prior to discharge (Discharge Screener version)
- At any visit (including intake) when the PHQ-9/A is positive. For example, if an individual scores positive on question 9 on PHQ-3 and/or scores in the moderate range or higher on PHQ-9, then the C-SSRS must be done.
- For children under 7 years old or an individual with intellectual disabilities, we use the C-SSRS Very Young Children full screen version.
If suicide risk is identified, a comprehensive assessment must be conducted and an action plan developed. A safety plan is completed with anyone who demonstrates risk but is not in need of immediate rescue and a copy of the safety plan is kept in the EMR record.
Assessment
Every client assessed to have suicidal risk receives a suicidal care management plan or pathway to care that is both timely and adequate to meet their needs. All nonclinical staff and ancillary team members, upon contact with a client who communicates suicidal thoughts by phone or in person, must immediately make a warm handoff (using their NAMI CONNECT skills) to a clinical provider to support and assess the individual.
Effective suicide care management plans include consultation, collaboration, and coordination among MHCGM staff, family/support system, and other care providers. Strategies to promote continuity of care are implemented to address those periods of highest risk, particularly for individuals who experience barriers to engaging in treatment. Strategies may include increased frequency of caring contacts, referral to the Care Transition Team, Intensive Transition Team, Rapid Response, peer support services, and any other measures to ensure safe transitions (i.e. warm handoffs between providers).
All suicide prevention documentation is contained within our EMR system.
Clinical Care Pathway for Suicide
When a client is evaluated and subsequently released to the community (i.e., not hospitalized), the assessing clinician coordinates an outreach call/caring contact within the following 72 hours to ascertain the client’s current status. Transitions in care include discharge from hospitals, including but not limited to the emergency department, or any situation in which a person at risk of suicide is between care providers.
A subgroup of our ZS Implementation Team has developed and piloted a Clinical Care Pathway for Suicide to ensure increased and frequent contact, regular re-assessment of risk, well-articulated safety plan, warm hand-off (live communication between care providers and releases of Information to support persons to maintain collateral contact.
Criteria for enrollment and disenrollment onto or off of the Pathway are below. Clinical judgement AND consultation with the supervisor of the treatment team would always accompany any of the options below.
Enrollment Criteria
- On the Columbia: “Yes” is selected on any question 2-5 or “Yes” for question 6 in the past 3 months.
- Hospital discharges for suicidal ideation/behaviors
- Cypress Center admissions with suicidal ideation/behaviors
- Any other time, with consultation, where there is risk present.
*A Columbia and a Safety Plan must be completed for anyone enrolled on the pathway
Disenrollment Criteria
- Clinical Judgement AND consultation would always accompany any of the options below:
- Consultation with treatment team, supervisor, and medical provider
- Zero (0) crisis contacts for suicidal ideation/behaviors within the last 3 months
- No hospital visits or admissions, including emergency room visits due to SI within the last 3 months.
- Engaged in treatment and using Safety Plan
- No suicide attempts, suicidal thoughts with intent and plan endorsed on progress notes within the last 3 months.
*Only Supervisors have access to disenroll a patient
Treat
In addition to targeting suicidal thoughts and behaviors, mental health treatment should also address co-occurring psychiatric symptoms. We treat individuals with both acute and chronic risk for suicide through a variety of interventions.
Based on the level of risk individuals are treated as follows:
When a patient is evaluated and subsequently released to the community (i.e., not hospitalized), the assessing clinician coordinates an outreach call/caring contact within the following 72 hours to ascertain the patient’s current status. Transitions in care include discharge from hospitals, including but not limited to the emergency department, or any situation in which a person at risk of suicide is between care providers.
90% of our patients who miss an appt are contacted within 8 hours to ensure safety and connection.
High acute risk: Individuals experiencing high acute risk for suicide typically require psychiatric hospitalization to maintain safety and aggressively target modifiable factors. These individuals need to be directly observed until they are on a secure unit and then located in an environment with limited access to lethal means (e.g., securing sharps, cords/tubing, toxic substances and other lethal means). During hospitalization co-occurring psychiatric symptoms should also be addressed and at discharge these individuals will be assigned to the Suicide Risk Care Pathway.
Intermediate acute risk: Individuals experiencing intermediate acute risk for suicide may require psychiatric hospitalization if related factors driving the risk are responsive to inpatient treatment (e.g., acute psychosis).If outpatient treatment is appropriate, the individual would be placed on the Suicide Risk Care Pathway and closely monitored using the interventions described above.
Low acute risk: Individuals experiencing low acute risk for suicide require outpatient management of suicide risk. These individuals may or may not need to be assigned to the Suicide Risk Care Pathway or may be temporarily assigned to the Pathway until further assessment of risk can be determined.
Chronic risk: Is also addressed and closely monitored for any changes that may indicate a shift to an acute risk state.
Safety Planning
Any patient who is seen in the ED, has a Rapid Response deployment, or answers “Yes” to any item on the C-SSRS screener receives the safety planning intervention.
For most adults, we use the Safety Planning Intervention developed by Stanley and Brown. The safety plan allows the patient to identify positive coping strategies, members of their support system, and important contact information for those whom the patient can call on if needed.
We recently implemented the Children’s Health Queensland Safety Plan(s) for children and caregivers which helps define age-appropriate strategies for the younger population and their caregivers. This can also be used with adults who experience intellectual challenges.
Key Outcomes
As noted above, since implementation of the Zero Suicide approach, MHCGM has accomplished the following:
- Decreased suicide deaths by an average of 33% compared with the 8 years prior.
- Trained 94% of staff in suicide prevention.
- Assessed suicide risk in 93% of active clients in 2024.
With regards to data collection, MHCGM has a Continuous Quality Improvement Plan where performance measures are tracked, reviewed and analyzed for the stability of the process. For example, at the end of each month, any patient who has had a suicide attempt but no safety plan on file, is flagged for follow-up with leadership.
For our Zero Suicide implementation, data is collected across our agency and is ever evolving. All trainings are recorded by our Continuing Educations Departments. Other information, including deaths by suicide, emergency department diversion rates, PHQ/C-SSRS ratings, and subsequent safety plans completed, etc., are currently being assessed for compilation into a Zero Suicide dashboard that will inform our targets for improvement. While we are early in the process of implementing Zero Suicide, we have collected the following data: 2018 marked our first full year of the Zero Suicide implementation. Below is the outcome data collected (see Table 1).
Table 1. Outcome Data
| OUTCOMES | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 |
|---|---|---|---|---|---|---|---|---|---|---|
| MHCGM DBT Program deaths by suicide | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mobile Crisis Response Team Emergency Dept diversion rate* | N/A | N/A | 90% | 94% | 98% | 98% | 91% | 81% | 83% | 84% |
Suicide Rate
When comparing suicide rates between 2018 and 2023 (the last year available as of publication), New Hampshire experienced a 23% decrease in suicide deaths (crude rate of 20.6 vs. 15.8). During the same period, MHCGM saw a decrease in patient suicides of 33%. It is important to note that Manchester constitutes NH’s diverse urban heart and is a federally designated resettlement zone. On average, data shows Manchester experiences poorer outcomes than 500 similarly urban areas, including but not limited to, elevated poverty rates, unemployment rates, and the rate of uninsured.
Training
The Zero Suicide Implementation Team regularly reviews the curriculum of suicide prevention trainings offered through MHCGM. When we began our implementation in 2018, we offered:
- Zero Suicide Foundations
- NAMI Connect Suicide Prevention/Intervention
- Counseling on Access to Lethal Means (CALM)
- Cognitive Behavioral Therapy for Suicide Prevention (CBT-SP)
- Columbia-Suicide Severity Rating Scale (C-SSRS)
- Crisis Intervention Training for law enforcement
- Safety Planning
- DBT, DBT-A, DBT for non-DBT clinicians
- CBT-SP
Since that time, we have enhanced our offerings to include Teachable Moment Brief Intervention (TMBI), L.E.T.S Save Lives (Listening, Empathy, Trust, Support), CALM-SAFE, Risk Formulation for Individuals Experiencing Psychosis. We are also exploring DBT-Sleep as insomnia is a critical factor in risk of suicide.
We have seen a reduction in deaths by suicide in our region, which we hope can be attributed, in part, to our community’s commitment to suicide prevention efforts and training.
As of 2024 82% of both clinical and nonclinical staff have received position-appropriate Zero Suicide-related training, including the following:
- Connect Suicide Prevention/Intervention
- Foundations of Zero Suicide: Clinical Competency
- Safety Planning
- Counseling on Access to Lethal Means (CALM)
- Dialectical Behavioral Therapy (DBT)
- Columbia-Suicide Severity Rating Scale (C-SSRS)
And because MHCGM is a regional leader in the evidence-based practices of Dialectical Behavioral Therapy (DBT), the suicide rate for clients receiving DBT has remained at zero.
Zero Suicide in the Community
Since 2016, MCHGM has offered a Mobile Crisis Response Team (MCRT) that provides 24/7 emergency assistance through the deployment of mental health clinicians and peer support/recovery coaches alongside law enforcement officers when needed.
Now part of a statewide Rapid Response system, MCRT has served thousands of individuals, providing tens of thousands of services to individuals of all ages with an average response time of 16 minutes. Currently, MCRT’s diversion rate away from the hospital emergency department and to appropriate mental and behavioral health services is 84%. In addition, our work with the Manchester Police Department has led to the implementation of Crisis Intervention Training (CIT).CIT is designed to enhance the strategic communication skills of police officers when responding to individuals experiencing behavioral health crises, thereby lessening incidences of force and reducing risk of injury.
CIT has revolutionized police and public interactions here in Manchester. Previously, an MPD Patrol Sargent stated to an NH expert reviewer that if MCHGM involvement with CIT and Mobile Crisis Response were to ever cease to exist, he would quit on the spot. MHCGM’s impact on the community, hospital diversions, suicide response, and overall cost savings for fire and safety services is immense.
In 2024, after noticing a trend in deaths by suicide involving bridges, MHCGM partnered with The City of Manchester and other provider agencies to implement signage on four of the city’s larger bridges where individuals had attempted or died by suicide. The signage includes a hopeful message and how to get help.
Caring for our Workforce
In 2023, a subgroup of our Zero Suicide Implementation Team developed and implemented procedures and a brochure for staff focusing on workforce suicide prevention. Emphasis was put on ensuring our staff know how to seek help if needed, along with how to identify signs of risk in co-workers. Additionally, a procedure was developed for managers, providing guidance on how they can compassionately respond in the event of a staff member experiencing a suicidal crisis.
While our workforce wellbeing efforts began in 2020 during the pandemic, we formalized our efforts in 2022 through the development of a Workforce Wellbeing team. Through this initiative we pay particular focus on upstream wellbeing strategies to prevent and manage burnout and to cultivate balance. A survey is conducted every 2 years to assess current needs and progress. We have also developed formal training on Cultivating Wellbeing and Trauma Stewardship to further emphasize the importance of caring for ourselves while doing critically important work.
Future Steps
Suicide prevention training will continue for existing staff and are required of incoming staff per our agency’s continuing education programming. It is the intention of MHCGM to continue to repeat the Zero Suicide workforce survey every 3 years. It is our hope to continue to gather relevant data around the impacts of training as well as staff competency and confidence in treating individuals experiencing suicidal ideation. We are working across our agency to ensure that all data is compiled intentionally and purposefully to drive positive changes in the delivery of care. Tracking the number of caring contacts, average response times, completion of suicide screenings and safety plans, and client satisfaction particular to this initiative will undoubtedly help all members of our community.
Because the targets of Zero Suicide require community investment, MHCGM will continue to engage partners in our efforts to create a suicide-safer healthcare system. With support from our Zero Suicide grant, we have strengthened our efforts and formalized our partnerships with the VA Medical Center and our local Healthcare of the Homeless program. We will continue to support our community partners in implementing the principles of Zero Suicide. Such partnerships include collaboration with training as well as systems to ensure pathways to behavioral health care.
Lastly, to further our community’s Zero Suicide implementation efforts, CIT trainings and recertifications are scheduled twice annually for Manchester police officers and for officers of surrounding areas. While MPD data analytics have yet to exist, officer anecdotes suggest that they now spend less time on mental health calls and feel more confident responding to calls when necessary. We also intend to participate in our state’s efforts to implement a standardized Postvention protocol.