Cambridge Health Alliance (CHA) serves residents of Cambridge and other communities north of Boston, Massachusetts. In 2023, the Alliance served nearly 130,000 patients at three hospitals and multiple care centers across the region. CHA primary care centers feature integrated behavioral health services and are staffed with psychiatrists, case workers, and psychologists. Inpatient psychiatric care is provided at all three CHA hospitals. CHA has a dual role in the community, as it also serves as the public health department for the City of Cambridge.
Suicide Care Journey Stories
SC CoIIN Objective
In joining the Suicide Care Collaborative Improvement and Innovation Network (SC CoIIN), CHA wanted to standardize suicide screening and assessment practices among clinicians. They also sought to prioritize the use of collaborative safety planning in patient care. Finally, CHA wanted to improve their communication with patients at risk of suicide after they were discharged.
Previous Experience with Suicide Care
Entering the SC CoIIN, CHA already had a number of suicide care practices and protocols in place. At the system level, CHA staff were trained on the health system’s suicide care protocols and responses. Staff received new training when processes were updated.
At the patient level, CHA nurses screened all admitted patients for suicide using the Columbia-Suicide Severity Rating Scale (C-SSRS).1 If the screen revealed that a patient was at risk for suicide, then a follow-up risk assessment was administered by either a physician or advanced practice registered nurse (APRN). With no timeline in place for this follow-up assessment, however, many were administered a few days after the initial screen. Finally, all patients who were at risk for suicide were supposed to leave CHA with a suicide safety plan upon discharge. In practice, though, this did not happen regularly.
Suicide Care Interventions Implemented
During their participation in the SC CoIIN, CHA made a number of changes designed to improve suicide care risk across the system, especially at the time of patient discharge.
1. Safety Planning
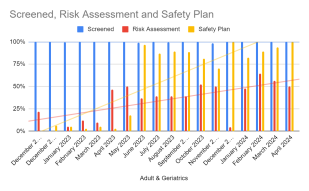
First, CHA wanted to improve the use of safety planning for patients who were at risk of suicide. Collecting data about the use of safety plans revealed a sobering finding: in December 2021, while 100% of adult patients in CHA were screened for suicide, none had a completed safety plan in place.
CHA reached out to the system’s social workers for advice on how to improve rates of safety planning. The social workers suggested that effective safety plans were a collaboration between a patient and a medical professional and were developed over time. CHA took that feedback and changed their process to begin conversations about safety planning at the time of admission, not discharge. Now, once a safety plan is created, the patient and clinician update it regularly. Clinicians also now review safety plans for all discharged patients who present as having a high risk for suicide.
“Working collaboratively with the social workers and trying to problem solve was helpful,” said Fiona McCaughan, an assistant chief nursing officer at CHA. “Having it be more of a co-production with the patient, rather than ‘see you later, you're being discharged, here’s this piece of paper with a plan,’ is what really made the difference.”
2. Data Reporting
Second, CHA changed their data reporting mechanisms. Originally, their report on safety planning included data from all patients in the system, including those who had screened negative for suicide risk—patients who would not need to complete a safety plan. CHA reworked their report to only collect data on discharged patients who had screened positive for suicide risk. With a new data collection plan in place, CHA was able to more accurately track rates of completed safety plans for patients who needed them.
3. Post-Discharge Connections
Finally, CHA sought to improve post-discharge connections to care in order to ensure that patients who were at risk of suicide continued to receive support. Key to this was improving access to follow-up appointments. All patients at risk of suicide scheduled a follow-up appointment with their clinician within one week after hospital discharge. However, many patients expressed difficulty finding transportation to that meeting and would end up not going. In order to deliver care to more people, CHA changed the follow-up procedure to allow patients to schedule the visits with social workers, nurses, and other staff at community behavioral health centers—many of which were easier for discharged patients to travel to.
Key Successes
CHA saw their rates of adult patients discharged with safety plans increase signficantly during their time in the CoIIN. In April 2023, only 2% of adults were discharged with safety plans. By March 2024, it was 94%.
Not only are more people benefitting from safety plans, but the collaboration between staff and patients has resulted in more connectedness.
“Staff regularly go in and talk to the patient, and the team will also give some feedback about items in the safety plan,” said McCaughan. “That has helped the staff get to know patients better.”
McCaughan also cited the increased use of data to drive decisions as a success for CHA. Providing actual safety plan and risk assessment data to clinicians was important, she says, because “nobody believes that they are at 0% for safety planning. Nobody believes that they could be doing the risk assessment on time only 16%. But digging into the data really helped.”
The CHA team is now using a data-driven approach to determine whether to continue having physicians or APRNs do the follow-up risk assessment for people who have screened positive for suicide risk, or whether it makes more sense for the nurse who does the initial screening to do the follow-up assessment immediately.
Lessons Learned
- Gathering data can be labor intensive, but it is important in driving organizational change.
- Communication among people who work different shifts is challenging and can be an obstacle to implementing new policies and protocols.
- Meeting regularly as a team fosters continuity and cohesion.
Opportunities for Future Suicide Safer Care
The CHA team identified opportunities for continued improvement after the conclusion of the SC CoIIN. At the top of the list is changing how CHA teaches staff about its suicide care pathway to ensure that all staff understand CHA’s protocols. The team is also going to continue testing changes and improvements to the post-hospitalization follow-up procedures with clients, including soliciting input on how safety plans are supporting clients’ needs.
- 1
Posner, K. (2007). Columbia-Suicide Severity Rating Scale (C-SSRS) [Database record]. APA PsycTests. https://doi.org/10.1037/t52667-000