Community Fairbanks Behavioral Health (CFBH) is part of Community Health Network, a large health care system serving central Indiana. CFBH offers a full range of behavioral health care, including inpatient, outpatient, and residential services across three different sites. The system has 160 beds and serves both youth and adult patients. CFBH serves nearly 13,000 patients in crisis each year.
Suicide Care Journey Stories
SC CoIIN Objective
CFBH supports the Zero Suicide approach to behavioral health care. With so many patients coming through the system annually, and with multiple departments involved in the care of these individuals, CFBH wanted to improve their suicide care pathway. This meant making sure that existing processes for suicide care were clear. CFBH also wanted to look for opportunities to improve their performance, especially regarding post-discharge follow-up and care.
“We have a lot of patients who come in with attempts of suicide, suicidal thoughts, and depression,” said Aimee Edmonds, director of acute clinical services at CFBH. “We wanted to make sure that we were providing the best care possible for that large population.”
Previous Experience with Suicide Care
After participating in a Zero Suicide Academy in 2014, CFBH fully implemented Zero Suicide in both ambulatory and acute settings. However, some of their Zero Suicide work was stalled when the grant that funded the work ended. The COVID-19 pandemic further challenged their organizational push toward Zero Suicide, as the system had to contend with other emergency health priorities, and some staff who had been leading the Zero Suicide work left the system.
Despite these challenges, CFBH had made progress toward their goal of Zero Suicide before the beginning of the Suicide Care Collaborative Improvement and Innovation Network (SC CoIIN). All CFBH caregivers had been trained in evidence-based screening and assessment tools, including the Columbia Suicide Severity Ratings Scale (C-SSRS)1 and Assessing and Managing Suicide Risk (AMSR).2 Collaborative safety planning between clinicians and patients was an established best practice, and clinicians strove to hold follow-up appointments with patients within seven days of discharge. However, CFBH staff wanted to improve communication during that week after discharge, which is an especially vulnerable time for people at risk of suicide.
Interventions Implemented
During their participation in the SC CoIIN, CFBH piloted a number of interventions designed to improve their suicide care pathway.
1. Improve post-discharge connections
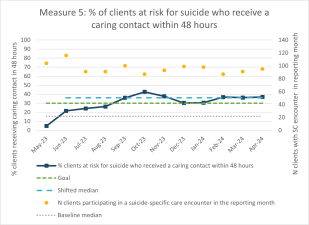
One of their first priorities was to improve connections with patients after discharge. In May 2023, CFBH conducted a Plan-Do-Study-Act (PDSA) cycle on a new Caring Contacts3 program, where they called five patients per month within 48 hours after discharge. During these conversations, Edmonds and another behavioral health care administrator asked patients about their plans to attend their follow-up appointment, as well as any barriers to continuing care they may have encountered.
The PDSA yielded helpful insights. Edmonds found that the communication was well-received by patients. She also learned that communicating by text was more efficient and effective than calling people directly, because people often would not answer their phones when called. As a result of this PDSA, CFBH has expanded the program to reach approximately 40 patients per month. They have also developed a brief text message script that asks patients about barriers to post-discharge care and provides them with the phone number for a clinician in the crisis department.
2. Safety planning
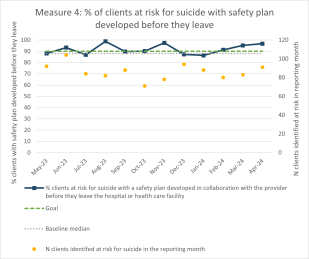
CFBH also worked to improve the safety planning process. Before the SC CoIIN, Edmonds noted that clinicians reported developing safety plans collaboratively with patients. However, electronic health record (EHR) data showed that approximately 20% of patients did not have a safety plan completed at the time of discharge.
When the team investigated the cause of this gap, they found that a flaw in the EHR system was to blame. Many clinicians were using an outdated safety planning tool that had remained in the EHR even after a new one was adopted. The data in the EHR pulled information from the new safety planning tool, not the one clinicians were using. This meant that not only was the data on completed safety plans inaccurate, but that many clinicians and patients were using an outdated safety planning process.
To ensure that collaborative safety planning continues to be a priority, CFBH has begun to audit safety plans as a part of the caring contact process. In an audit, clinicians review a discharged patient’s chart to make sure that their safety plan is complete and documented, and that it was reviewed with a family member or other support person. Findings are discussed with the therapist team during their weekly huddle.
Key Successes
As a result of their caring contacts work, CFBH is now reaching significantly more patients post-discharge than they were before participating in the SC CoIIN. In May 2023, caring contacts were simply not happening. But by December 2023, CFBH had achieved its goal of reaching at least 30% of patients at risk for suicide with a caring contact within 48 hours after discharge.
CFBH’s work during the SC CoIIN also highlighted the importance of bringing people with lived experience into conversations about the system’s suicide care. The SC CoIIN provided the motivation for CFBH team members to reach out to previous patients and family members who had expressed interest in supporting CFBH’s suicide care work. To better integrate the voices of people with lived experience into the system’s suicide care pathway, CFBH created a new Patient and Family Advisory Council, which will advise CFBH on issues related to acute and crisis care. The council’s first meeting took place in May 2024.
“In our clinical meetings, we would always say that it would be nice to have people with lived experience involved in our work,” says Edmonds. But with many competing priorities, no action was ever taken. “The SC CoIIN motivated us. We said, ‘Okay, this is a really good idea to involve lived experience. Let’s really try to make it happen.’”
“The SC CoIIN motivated us. We said, ‘Okay, this is a really good idea to involve lived experience. Let’s really try to make it happen.’”
Lessons Learned
- Time is always a challenge, especially when trying to coordinate meetings between clinicians and administrators. Offering team meetings at different times during the day helped to bridge some of those timing conflicts.
- Patients and families want to support suicide care efforts. Partnering with them can provide new insights.
- Text messaging is a more effective way of reaching patients after discharge than calling.
Opportunities for Future Suicide Safer Care
CFBH continues to refine and improve their suicide care pathway, especially with respect to caring contacts. They are working on a text messaging system that automatically sends a scripted message to all patients with a safety plan within 48 hours after discharge. They also plan to gather data on whether these communications result in better patient attendance at post-discharge appointments. Finally, to further the progress they made in the SC CoIIN, CFBH has recently formed a team to focus on Zero Suicide trainings and policies.
- 1
Posner, K. (2007). Columbia-suicide severity rating scale (C-SSRS) [Database record]. APA PsycTests. https://doi.org/10.1037/t52667-000
- 2
Education Development Center. (2019). Assessing and managing suicide risk: Core competencies for health and behavioral health professionals working in inpatient settings.https://solutions.edc.org/solutions/zero-suicide-institute/amsr/curricula/amsr-inpatient
- 3
Motto, J. A., & Bostrom, A. G. (2001). A randomized controlled trial of postcrisis suicide prevention. Psychiatric Services, 52(6), 828–833. https://doi.org/10.1176/appi.ps.52.6.828