Trinity Health Grand Rapids (THGR), part of Trinity Health system in Michigan, is a Joint Commission-accredited teaching hospital that includes the Lacks Cancer Center, Hauenstein Neuroscience Center, Emergency and Trauma Services, Orthopedic Center of Excellence, Wege Center for Health and Learning, and the area’s premier primary care network, Trinity Health Medical Group. In addition to implementing Zero Suicide practices as part of the Suicide Care Collaborative Improvement and Innovation Network (SC CoIIN), THGR’s behavioral health continuum includes a Behavioral Health Crisis Center, adult inpatient medical psychiatric care, and recovery medicine for substance use disorders.
Suicide Care Journey Stories
SC CoIIN Objective
THGR joined the SC CoIIN with the objective of moving toward more person-oriented care in its psychiatric medical unit, primary care settings, emergency departments, and inpatient medical units. THGR wanted to expand beyond focusing on the patient’s actual stay in the hospital to take into consideration the patient’s life situation before hospitalization, and transition planning and follow-up after the hospital stay.
THGR also wanted to establish a clear suicide care pathway for patients entering its health care system by focusing on the five primary drivers of the SC CoIIN project: respectful, compassionate care; skilled and activated hospital staff; standardized screening and assessment practices; collaborative, person-centered care planning; and supportive and timely care transition.
“It’s a very lonely journey for people who are dealing with suicidal ideation,” said Casie Sultana, a clinical nurse leader in behavioral health. “We want to be a place where they feel welcome and comfortable seeking help.”
Previous Experience with Suicide Care
Before the SC CoIIN, THGR mainly focused on ensuring the hospital environment was safe. It did not collect data on suicide care screening, assessment, and treatment, and its suicide risk assessment and safety planning were not standardized. Although there was suicide care training for clinical staff, other frontline staff were not prepared to screen patients for suicide. THGR also did not provide consistent, continuous contact or support post-discharge for people identified as at risk for suicide.
Interventions Implemented
THGR implemented several interventions during the SC CoIIN that have improved its suicide care.
1. Standardized assessment practices
THGR standardized its documentation practices for the Suicide Assessment Five-Step Evaluation and Triage (SAFE-T) risk assessment.1 If a patient’s risk for suicide was moderate or high on the SAFE-T risk assessment or if a patient came in with a primary reason of suicidality or self-harm, suicide risk was considered a primary concern rather than secondary as it was before the SC CoIIN.
2. Safety planning
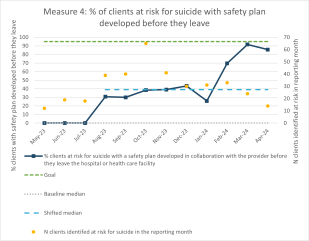
Another key intervention was introducing a standardized safety planning tool: the Stanley-Brown Safety Plan.2 THGR used this tool with all patients identified at moderate or high risk for suicide in one medical unit and one psychiatric medical unit so that patients would be better prepared to leave the hospital. In May 2023, THGR reported that 0% of patients at risk of suicide had developed a collaborative safety plan before discharge. By March 2024, 90% of clients had one in place. THGR will be implementing this tool in all the other departments during the summer of 2024.
3. QPR training
Inspired by Trinity Ann Arbor’s use of QPR (Question, Persuade, Refer),3 THGR is now training its trainers to implement QPR for staff. The training will improve the screening process, including how the staff ask the screening questions. It will also help staff discuss suicide with patients and encourage patients to seek help.
Key Successes
THGR has switched its focus to the whole patient, including what brought them to the hospital and what their care will include after they are discharged. Partway through the SC CoIIN, to help move toward this outcome, THGR changed team members and added the leader of outpatient social work. These changes have been vital to understanding the work on the outpatient side of THGR’s health care system and learning ways it can improve the transitions for patients.
A major improvement has been the percentage of patients experiencing suicidality who completed the Stanley-Brown Safety Plan before being discharged from care. That percentage increased from about 30% in August 2023 to 91% in March 2024. Implementing this safety plan as a standardized practice is very important for supporting patients after they are discharged from the hospital.
“This safety plan aims to mitigate risk and has been a great tool helping me work with patients more closely and develop safe discharge plans,” said Kristen Ranson, a licensed social worker. “I'm excited to roll this out to the other social workers in the department so they can start using it.”
THGR also implemented a standardized method for collecting medical information and documentation in the electronic health records (EHRs), including the SAFE-T risk assessment results. This change will enable THGR to enter data into the EHR to help improve care by making it more obvious to the clinical staff what the risk level is and what interventions need to be put into place to provide a safe environment for each patient.
Working together, THGR, Trinity Health Ann Arbor, and Trinity Health Syracuse were also able to get standardized documentation implemented in EHRs across the Trinity Health System nationally. Members from the three health care systems advocated for implementation of this change to promote the spread of what they found to be a best practice. They took the proposed changes through the Trinity Health National Behavioral Health Clinical Excellence Council for support and approval. Being part of the SC CoIIN prepared the three sites to speak to the benefit of a standardized suicide assessment in the EHR.
Lessons Learned
- Be thoughtful about who needs to be at the table in making decisions. Involve the key partners from the beginning.
- Pay attention to who owns and leads the project. It is important to have leaders who have the time to make this type of project a priority. It takes a lot of time and effort to determine the changes that need to be made, how to make them, and then implement and evaluate them.
- Due to a low response rate, surveys were not successful in getting feedback from patients about whether changes in care were helping them. Some success did occur when a staff leader talked directly with patients at their bedside. However, it was hard to fit this into the staff’s day-to-day work. THGR will continue trying to determine the best way to get useful patient feedback.
“In our day-to-day work there are always things you can cancel and move to the bottom of your list. But if you do that with this work, you will never get anywhere with it,” said Susan Burchardt, a clinical services manager in care coordination. “This has to be at the top of your priorities.”
Future Opportunities
Overall, THGR wants to continue to create an optimal suicide care pathway by implementing the changes piloted at the two SC CoIIN units across the entire system. These changes include taking a whole patient approach to care, adopting the Stanley-Brown Safety Plan, and using standardized documentation in the suicide care pathway. THGR also plans to provide QPR training to all staff.
With Zero Suicide as a goal, THGR plans to improve how it obtains feedback from patients about suicide care so that it can make improvements. It wants to increase the rate of safety plan use and implement caring contacts for patients after they have left the unit. Finally, THGR is sharing its achievements with other Trinity Health hospitals in its system, with the goal of sharing what works for safer suicide care.
- 1
U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. (2009). SAFE-T: Suicide Assessment Five-Step Evaluation and Triage.
- 2
Stanley, B., & Brown, G. (2012). Safety Planning Intervention: A brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256–264.
- 3
Quinnett, P. (2013). QPR gatekeeper training for suicide prevention: The model, theory and research. QPR Institute. https://www.researchgate.net/publication/254002929_QPR_Gatekeeper_Training_for_Suicide_Prevention_The_Model_Rationale_and_Theory